This is an automatically translated article.
Cellulitis is a bacterial skin infection that can occur in almost any part of the body but mainly the legs and is characterized by painful swelling and redness of the skin. In addition, this bacteria can enter the bloodstream and lymph nodes and become life-threatening if it is not treated quickly. This article will introduce the treatment of cellulitis of the legs
1. Cellulitis?
Cellulitis, also known as cellulitis, is a fairly common bacterial skin infection that can occur in almost any part of the body. Cellulitis in the legs is most common, but it can also occur in the neck, face, or arms. Usually, the disease is only present on one side such as cellulitis of the left leg or cellulitis of the right leg. Rarely, cellulitis of the foot occurs in both legs simultaneously.
Characteristic of cellulitis is painful swelling and redness on the affected skin and usually does not cause an abscess or pus discharge.
In cellulitis of the lower leg, there are often manifestations such as tight, shiny skin, swelling, and rapidly developing skin sores/rash. The affected area may feel warm and there may be an abscess with pus around the infection.
2. What causes cellulitis in the legs?
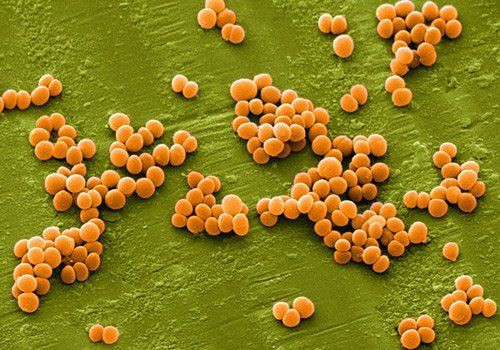
Cellulitis is an infection caused by bacteria, usually beta-hemolytic streptococci (Streptococcus pyogenes), followed by methicillin-susceptible Staphylococcus aureus. These bacteria usually do not cause problems when in contact with normal, healthy skin. However, open wounds or cracks in the skin can allow bacteria to penetrate deeper layers of the skin, causing swelling and other symptoms in the affected skin. Bacteria can enter the skin through any site of a wound or stretch mark such as:
Recent surgical wound Cuts Perforated wounds Athlete's feet Skin irritation Animal bites Skin thinning due to swelling or dryness

Bệnh viêm mô tế bào cẳng chân có thể do một số chấn thương gây ra
3. Who is at risk for cellulitis in the lower leg?
Cellulitis is relatively common, and most commonly occurs in middle-aged and older people. Although cellulitis can affect anyone, people with certain physical conditions are more susceptible to infection than others. Here are some factors that can put you at higher risk of cellulitis in your feet:
Skin trauma after surgery, broken bones, accidental cuts or burns. Any disease that weakens the body's ability to fight infection. People with diabetes, AIDS, or leukemia are often at higher risk of bacterial infections. Use of drugs that weaken the immune system. Swollen leg after surgery. Obesity History of cellulitis in the legs Poor blood circulation leads to skin that is susceptible to damage and infection.
4. Diagnosis of cellulitis?
Currently there is no gold standard to confirm the diagnosis of cellulitis, which is usually based on symptoms and medical history. Specifically, cellulitis is diagnosed based on the presence of widespread erythematous dermatitis in the deep dermis and subcutaneous tissue of the lower leg (cellulitis of the lower leg). It is characterized by increasingly severe erythema, edema, heat, and pain. Two of the four criteria (heat, erythema, edema, or pain) are required for diagnosis. The most common manifestation of the disease is in the lower legs, but it can affect any part of the body.
In addition, the patient's skin is also thoroughly evaluated for potential causes of cellulitis by looking for minor skin wounds following trauma, insect bites, pressure sores or injection site. If the patient has cellulitis of the lower leg, careful evaluation should be made to see if there are cracks or tinea versicolor in the feet. In addition, the disease can affect the lymphatic system and cause swollen lymph nodes underneath. Edema associated with cellulitis can lead to vesicle formation, swelling around the hair follicles leading to pox.
Blood cultures should be considered in immunocompromised patients, trauma from immersion, or animal bites. Blood cultures are also needed when the patient has signs of systemic infection.

Hình ảnh viêm mô tế bào cẳng chân với triệu chứng viêm da ban đỏ lan rộng
5. How to treat shin cellulitis?
Cellulitis of the lower leg is curable with prompt treatment with appropriate antibiotics. However, if not treated promptly, the bacteria can enter the bloodstream and lymph nodes and become serious and life-threatening.
5.1. Antibiotic therapy Patients with mild cellulitis and no signs of systemic infection should be covered with antibiotics targeting streptococcal therapy. The duration of treatment with oral antibiotics should be for a minimum of 5 days. In nonpurulent cellulitis, patients should receive cephalexin 500 mg every 6 hours. If the patient has a severe allergic reaction to a beta-lactamase inhibitor, then clindamycin 300 mg to 450 mg every 6 hours should be treated.
In patients with purulent cellulitis, methicillin-resistant Staphylococcus aureus, abscess-associated cellulitis or extensive perforation, or a history of intravenous drug use, the patient should also antibiotics against methicillin-resistant Staphylococcus aureus. Cellulitis with risk factors for methicillin-resistant Staphylococcus aureus should be treated with trimethoprim-sulfamethoxazole 800 mg/160 mg twice daily for 5 days along with cephalexin 500 mg every 6 hours. If the patient is allergic to trimethoprim-sulfamethoxazole, treat with clindamycin 300 mg to 450 mg every 6 hours. A longer duration of antibiotic therapy may be considered in patients who show minimal improvement with antibiotic therapy within 48 hours.
Hospitalization for systemic antibiotics may be necessary for patients who:
have signs of systemic infection (present two or more of the criteria for systemic inflammatory response: fever (above 38°C) ), tachycardia (heart rate over 90 beats/min), tachypnea (respiratory rate over 20 beats/min), leukocytosis (white blood cell count above 12000/mm), leukopenia (white blood cell count less than 4000/mm), or bleeding greater than or equal to 10%. ), unsuccessful outpatient treatment, Immunodeficiency, Rapidly progressive erythema, Intolerability to oral drugs, Intravenous antibiotics should be started to counteract Group A streptococci. Patients without risk factors for methicillin-resistant Staphylococcus aureus should be treated with intravenous cefazolin and, when possible, switched to cephalexin for a total of 5 days of treatment. If risk factors for methicillin-resistant Staphylococcus aureus are present, initiate treatment with vancomycin then de-escalate to trimethoprim/sulfamethoxazole.
In immunocompromised patients requiring hospitalization for parenteral antibiotic therapy, broad-spectrum antibiotic coverage with vancomycin plus piperacillin-tazobactam or carbapenem may be necessary.
5.2. Wound care This is an important part of cellulitis treatment. Covering the skin will help the wound heal. If you need a special dressing or dressing, you will be taught how to apply and change the dressing.
5.3. Rest Proper rest can help prevent cellulitis in your legs from becoming severe and help your body heal.
5.4. Elevate your feet If you have cellulitis in your feet, elevating your feet can help reduce swelling and help you heal.
5.5. Medications Use over-the-counter pain relievers such as acetaminophen or ibuprofen to relieve pain and reduce fever.
Thus, cellulitis of the foot is a common disease. If cellulitis is treated promptly, it usually clears up with appropriate antibiotic treatment. However, if not treated promptly, the bacteria can enter the bloodstream and lymph nodes and become serious and life-threatening.
If the above methods do not improve your condition, visit a medical facility, the doctor will examine and indicate the most useful treatment for you. Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading doctors, modern equipment and technology, but also stands out for its examination and consulting services. and comprehensive, professional medical treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.