This is an automatically translated article.
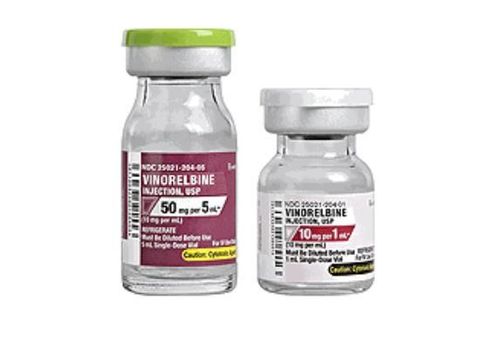
Grafeel drug is made in the form of an injection solution with the main ingredient of the drug is Filgrastim 300mcg/ml. So what is the effect of the drug Grafeel and how to use it?
1. What are the effects of Grafeel?
The main ingredient of Grafeel is Filgrastim, which is a human granulocyte colony-stimulating factor (G-CSF). This active substance is produced by recombinant DNA technology, has the same activity as the endogenous factor that stimulates the human granulocyte flow. Grafeel regulates the production and mobilization of neutrophils from the bone marrow. Grafeel also stimulates the activation, proliferation and differentiation of neutrophil progenitor cells. In some cases of chronic neutropenia, treatment with Grafeel also increases the production of eosinophils and basophils. Agranulocytosis is directly dependent on the dose of Grafeel.When Grafeel treatment was discontinued, circulating neutrophils decreased by 50% within 1-2 days and returned to normal within 1-7 days.
Grafeel is indicated in the following cases:
Grafeel is used to shorten the duration of severe neutropenia and complications in the following cases: The patient is receiving cytotoxic chemotherapy, this are the types that commonly cause febrile neutropenia. A patient on myelosuppressive therapy preparing for a bone marrow transplant. Long-term use of Grafeel increases the neutrophil count and reduces the frequency and duration of infections in patients with: Congenital neutropenia. Cyclic leukopenia. Idiopathic neutropenia, with a neutrophil count ≤ 0.5 x 109/l and a history of severe or recurrent infections. Drug-induced leukopenia. Cancer is not caused by bone marrow cells. Grafeel is contraindicated in the following cases:
People who are allergic to any of the ingredients of Grafeel. Note when using Grafeel drug in the following cases:
The safety of Grafeel drug for pregnant women has not been established. The use of Grafeel in pregnant women should be weighed against the benefits of treatment. It is not known whether the Filgrastim in Grafeel is excreted in human milk. Grafeel is not recommended for use in nursing women.
2. Dosage and how to take Grafeel
In patients receiving chemotherapy for a non-myeloid malignancy, the recommended dose of Grafeel is 0.5MUI (5mcg/kg corresponding to 16.6 microlitres of injection solution) injected once daily.
For patients treated with cytotoxic chemotherapy and autologous bone marrow transplantation, the starting dose of Grafeel is 1MUI (10mcg/kg/day) by continuous subcutaneous infusion over 24 hours or 1MUI (10mcg/day) kg/day) by continuous intravenous infusion over 30 minutes or over 24 hours. Grafeel medicine needs to be diluted in 20ml of 5% glucose infusion.
Once the patient has passed the lowest neutropenic threshold, the daily dose of Grafeel should be adjusted according to the response of the neutrophil count as follows:
The neutrophil count > 1.0 x 109/l for 3 consecutive days, adjust Grafeel dose to 0.5MUI (5mcg)/kg/day (corresponding to 16.6 microlitre injection solution/kg). Then, if the absolute neutrophil count remains >1.0 x 109/l for another 3 consecutive days, discontinue the drug. If the absolute neutrophil count falls <1.0 x 109/l during treatment, the dose of Grafeel should be increased again in the same increments as above. Grafeel has been shown to be effective and well tolerated when treated as above at doses up to 7.0MUI (70mcg/kg/day).
For patients with chronic severe leukopenia, Grafeel is used as follows:
Initial dose: Congenital leukopenia: 1.2 MUI (12 mcg)/day, divided into one or more times. Spontaneous or periodic leukopenia: Use a dose of 0.5MUI (5mcg/kg/day), divided into one or more times. Dose adjustment: The dose of Grafeel should be individualized and should be ensured to maintain a minimum neutrophil count of 1.5 x 109/l. Long-term daily dosing of Grafeel is indicated to achieve the required neutrophil count. The dose of Grafeel may be increased if the neutrophil count has not reached 1.5 x 109/l after 2 weeks of treatment, and the Grafeel dose should be reduced by half if the granulocyte count has increased by more than 10 x 109/l. The dose of Grafeel should be increased rapidly in patients with severe infections. Doses of Grafeel in excess of 14.5 MUI (145 mcg/kg/day) should only be used when it is known with certainty that the patient can tolerate it. The way to take Grafeel is as follows:
Grafeel can be used by subcutaneous or intravenous infusion for a short time, diluted in 5% Glucose solution infused over 30 minutes. The first dose of Grafeel should not be used earlier than 24 hours after the end of cytotoxic chemotherapy. The daily dose of Grafeel should be continued until the patient has passed the lowest stage of neutropenia, and the neutrophil count has reached normal levels. The time required for treatment with Grafeel can be up to 14 days depending on the type, dose and cytotoxic chemotherapy regimen previously administered. In patients receiving cytotoxic chemotherapy, a temporary increase in neutrophil counts usually occurs 1-2 days after starting Grafeel. However, for a more prolonged response to therapy, patients should continue treatment with Grafeel until the period of maximal leukopenia has passed or until the neutrophil count has returned to normal. normal. For patients receiving cytotoxic chemotherapy and autologous marrow transplantation: Grafeel can be administered subcutaneously or intravenously, by dilution in 20-50 ml of 5% Glucose solution. The efficacy and safety of Grafeel taken for more than 28 days have not been established.
3. Grafeel drug side effects
Taking Grafeel at the recommended dose usually causes mild to moderate musculoskeletal pain, in about 20% of patients. These symptoms, however, are sometimes severe, but are usually controlled with standard pain medications. Less common side effects of Grafeel include urinary abnormalities, mainly mild to moderate dysuria. There has been occasional transient decrease in blood pressure with the use of Grafeel, which does not require clinical treatment. Elevations of lactate dehydrogenase, serum uric acid, alkaline phosphatase, and glutamyl transpeptidase may occur but are usually mild to moderate, dose dependent and reversible. WBC counts above 100 x 109/l occurred in approximately 5% of Grafeel-treated patients at doses >0.3 MUI/kg/day (3 mcg/kg/day). However, no adverse effects directly related to this leukocytosis were observed. In clinical trials, Grafeel did not increase the incidence of adverse effects of cytotoxic chemotherapy. Adverse events occurring in patients treated with Grafeel in combination with chemotherapy included nausea and vomiting, hair loss, headache, fatigue, anorexia, diarrhea, mucositis, cough, skin redness, chest pain, sore throat, generalized muscle weakness, constipation, and nonspecific pain. Vascular disorders such as veno-occlusive disease and fluid volume disturbances have occasionally occurred in patients treated with high-dose chemotherapy followed by autologous marrow transplantation. In animal toxicity studies, Grafeel caused irreversible intracerebral hemorrhage that was observed in monkeys.
4. Grafeel drug interactions with other drugs
Grafeel should not be diluted with saline solutions. Above is important information about Grafeel medicine, patients should learn carefully about the use of the drug and consult a doctor, pharmacist to make the process of taking the drug more effective.