This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Inflammatory bowel disease is a part of inflammatory bowel disease, Enteritis is a term used to describe general inflammation in the intestines caused by both bacteria and viruses. If inflammation occurs anywhere in the digestive tract, it disrupts the function of the organs, causing pain and life-threatening.
1. Joint manifestations of inflammatory bowel disease
Among the extra-gastrointestinal manifestations of inflammatory bowel disease, those affecting the musculoskeletal system are among the most common, and have been reported in a number of series affecting 6 through 46% of patients. Idiopathic arthritis has been considered a disease group grouped under the heading 'spondyloarthritis' (SpA), also in this category are psoriatic arthritis, ankylosing spondylitis and reactive arthritis. .
Increasing understanding of the immunophysiology of these conditions, highlighting common changes in immune and inflammatory responses common to diseases with potentially diverse clinical manifestations . In addition, an increasing number of treatment options are available for patients with spondylolisthesis, with some agents being more or less effective for specific manifestations. Several agents used to treat spondylolisthesis have also been shown to be effective in inflammatory bowel disease, highlighting some of the common aspects of immunoregulatory dysregulation in these conditions.

Bệnh viêm ruột có thể gây viêm dính cột sống
2. Why can inflammatory bowel disease cause joint damage?
Rheumatic manifestations in patients with inflammatory bowel disease have been hypothesized to be due to activated intestinal lymphocytes in the joints and around the joints; These data suggest the presence of an 'enteric spine'. In patients with inflammatory bowel disease, lymphocytes of various subtypes can access joint sites using a variety of adhesion molecules and their antagonistic receptors. In addition to abnormal lymphocyte migration, dysbacteriosis, or altered gut microbiota diversity, there may be another common pathophysiological mechanism between inflammatory bowel disease and rheumatoid arthritis. related to inflammatory bowel disease.
3. Arthritis of the spine (the axial system of the body)
Spinal involvement is a common feature of inflammatory bowel disease arthritis. Typical symptoms are back pain caused by inflammation; Other features of ankylosing spondylitis have been well demonstrated in patients with inflammatory bowel disease-associated arthritis. These features are more commonly observed in patients with Crohn's disease (5-22%), compared with ulcerative colitis (2-6%)
Viêm khớp cột sống là bệnh viêm khớp do bệnh viêm ruột gây ra
4. Clinical features of ankylosing spondylitis in patients with inflammatory bowel disease
Inflammatory back pain is characterized by dull back pain of onset, lasting more than three months, associated with morning stiffness and improving with exercise. Ankylosing spondylitis has traditionally been diagnosed based on a combination of symptoms of inflammatory back pain, limited spinal flexion (Schober test), and decreased thoracic compliance and radiographs. suggests bilateral sacroiliitis or unilateral sacroiliitis.
There seems to be a genetic link between ankylosing spondylitis and inflammatory bowel disease. Approximately 5-10% of patients with ankylosing spondylitis develop inflammatory bowel disease, and up to 70% of patients may have microscopic evidence of enteritis; Likewise, about 5-10% of IBD patients may develop ankylosing spondylitis. The presence of elevated C-reactive protein and serum and/or fecal calprotectin in patients with ankylosing spondylitis has been shown to have modest accuracy as a screening strategy for identifying inflammatory patients. Potential ankylosing spondylitis with enterocolitis.
Most ankylosing spondylitis patients are positive for HLA-B27. Patients with inflammatory bowel disease and ankylosing spondylitis have a much higher positivity rate for HLA-B27 than the general population (∼50%) but lower than patients with ankylosing spondylitis. Regarding the diagnosis of hip arthritis, magnetic resonance imaging (MRI) is often considered the gold standard. X-ray changes are often more specific for ankylosing spondylitis, but are less sensitive.
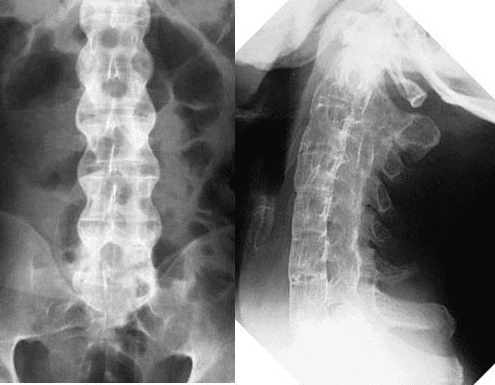
Hình ảnh X quang của bệnh nhân viêm cột sống dính khớp
5. Other musculoskeletal extraintestinal manifestations of inflammatory bowel disease
Besides peripheral joint and spinal diseases, enteritis, tenosynovitis, and tenosynovitis are commonly observed, especially if highly sensitive imaging techniques such as ultrasound are used.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Arthur Kavanaugh, Abha Goyal Singh, Rheumatologic Complications of Inflammatory Bowel Diseases, Dispatches from the guild conference, series
4, practicalgastro. Ott C, Schölmerich J. Extraintestinal expressions and complications in inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2013;10:585-95 Colia R, Corrado A, Cantatore FP. Rheumatologic and extraintestinal manifestations of inflammatory bowel diseases. Ann Med. 2016;48:577-58 Vavricka SR, Schoepfer A, Scharl M, et al. Extraintestinal Manifestations of Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:1982-92 Olivieri I, Cantini F, Castiglione F, et al. Italian Expert Panel on the management of patients with coexisting spondyloarthritis and inflammatory bowel disease. Autoimmun Rev. 2014;13:822-30 Molodecky NA, Soon IS, Rabi DM, et al. Increasing prevalence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2011;142:46-54