This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.It is believed that ulcerative colitis may be primarily determined by a complex combination of environmental and host factors, genetic variations, immune responses, and gut microbiota. The onset of this disease is triggered by disturbances of the mucosal barrier, intestinal microbiota, and an abnormal immune response.
Many scholars support that the abnormal immune response (innate and adaptive) is an important direct pathogenesis mechanism, in which the gut microbiota is an important stimulus for damage. This immune injury and environmental and host factors may be causative factors.
1. Environmental factors and hosts
It has been recognized that environmental and host factors play an important role in increasing the susceptibility of developing ulcerative colitis. The increasing incidence of ulcerative colitis worldwide demonstrates the importance of environmental factors in the progression of this disease.
This is similar to the pattern discovered in the Western world in the early 20th century. Ulcerative colitis especially occurs in urban areas and its incidence is faster and then slower. . Westernization and accompanying urbanization, sedentary lifestyle, exposure to environmental pollution, dietary changes, antibiotic use, refrigeration, better hygiene, and fewer infections are considered. are contributing factors.
For example, former cigarette smoking has been reported to be one of the strongest risk factors for ulcerative colitis, whereas compared with former smokers and non-smokers, active smokers have less ulcerative colitis and they predominantly present with a milder clinical course. In addition, appendectomy is considered to have a protective effect on the future development of ulcerative colitis.
2. Genetic Variations
Primarily genetic studies are effective in recognizing both common and infrequent genetic variants associated with susceptibility to ulcerative colitis. Human leukocyte antigen and adenylate cyclase type 7 are two important ulcerative colitis-specific genes. Furthermore, many ulcerative colitis-specific genes were confirmed to be responsible for mediating epithelial barrier function. However, ulcerative colitis and Crohn's disease share most of the same genetic factors. These shared genetic factors can encode cytokines, innate and adaptive immune signaling pathways, and immune sensing, such as interleukin (IL)-10, -12, -23R and region caspase recruitment contains the protein 9.
In addition, it has been shown that about 70% of genetic variants are also commonly seen in several other autoimmune diseases, such as ankylosing spondylitis and psoriasis. Overall, genetic factors intentionally increase susceptibility to ulcerative colitis in a small but definite manner. However, many individuals do not exhibit genetic susceptibility when all susceptibility loci are assessed by polygenic risk scores. These findings imply that an abnormal adaptive immune response and epithelial barrier dysfunction may play important roles in the pathogenesis of ulcerative colitis.
3. Intestinal microbiota
A series of animal experiments and clinical trials have confirmed the presence of significant intestinal dysbiosis in patients with ulcerative colitis. The gut microbiota dysbiosis is characterized by reduced biodiversity, irregular composition of the gut microbiota, and altered spatial distribution, along with microbiota interactions. owner. There was a significant change in gut microbiota in patients with ulcerative colitis as reflected in a decrease in probiotic bacteria (eg, Bifidobacterium and lactobacillus, etc.) conditions (such as Enterococci and Enterobacteria, etc.). Therefore, more and more studies are paying attention to the therapeutic effect of fecal microbial transplantation from healthy donors in patients with ulcerative colitis.
4. Immune system ulcerative colitis is an inflammatory disease mediated by the immune system
Innate immunity is the first line of defense against pathogens. Unlike adaptive immunity, innate immunity is nonspecific and long-lived. Immune cells in innate immunity, such as dendritic cells (DCs), macrophages, natural killer cells, intestinal epithelial cells, and fibroblasts. Being able to sense the gut microbiome and respond to conserved structural patterns of microorganisms, can trigger an effective rapid inflammatory response and prevent bacterial colonization. Among them, DCs are specialized antigen-presenting cells responsible for T-cell activation and the induction of adaptive immune responses, which play an important role in the interaction between immunity and the immune system. innate and adaptive translation.
For the adaptive immune system, the components of this system work together with each other, with molecules and with cells in the innate immune system to produce an effective immune response that eliminates remove invading pathogens under normal conditions. Unlike innate immunity, adaptive immunity is highly specific for a long time and is adaptive because antigen specificity is the result of complex maturation and development of immune cells. Translate . Helper (Th) cells are key factors for the adaptive immune response. Ulcerative colitis is primarily triggered by an immune response induced by Th2 cells. Th2 cells are mainly induced by IL-13 and subsequently secrete IL-4, IL-5 and IL-13, of which IL-13 is considered essential for the pathogenesis of ulcerative colitis.
5. Pathophysiology of upper gastrointestinal tract lesions
The pathogenesis of upper gastrointestinal mucosal lesions has not been elucidated. However, many researchers support that it is similar to the colonic lesions of ulcerative colitis. Cellular immune responses to certain bacteria may contribute to the potential pathogenesis of ulcerative colitis. Interestingly, similar immune molecules were also demonstrated in both upper gastrointestinal and colon tissues (Figure 4). For example, a previous study suggested that Th2 cells activated by CCR3+ and Crohn's disease 62L in the upper gastrointestinal tract may originate from mucosal lesions of the colon. Furthermore, Berrebi et al. reported that the chemokine receptor CXCR3 was uniformly expressed in the epithelium and stroma of the perivascular regions of gastric biopsies from patients with ulcerative colitis. While the chemokine receptor CCR5 is found in lymphocytes around the stroma. Therefore, an increase in the lymphocyte population upon stimulation in the colon of patients with ulcerative colitis may lead to a lymphocytic infiltration in the stomach. Furthermore, an excessive autoimmune response to bacterial antigens caused by genetic susceptibility to aberrant immune responses can lead to the incorporation of memory T cells in the mucosa. colon in the upper gastrointestinal tract. However, there is no relevant evidence on the correlation between H. pylori and peptic ulcer.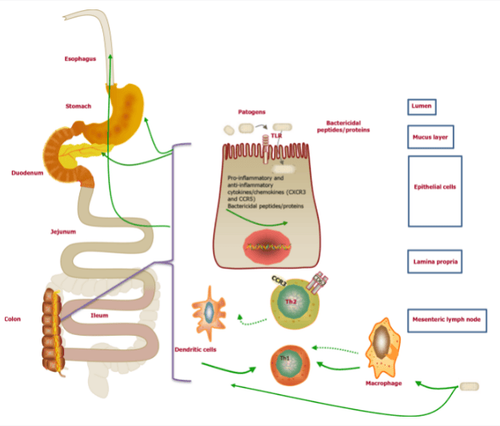
6. Molecular Pathological Epidemiology
Molecular pathological epidemiology (MPE) has been reported to be an integrated transdisciplinary science that integrates the disciplines of molecular pathology and epidemiology. Unlike conventional epidemiological research, such as genome-wide association studies, molecular pathological epidemiology primarily explores the underlying heterogeneity of disease processes. While traditional molecular epidemiology often treats disease as a single entity. Similar to biological systems and WebMed, molecular pathological epidemiology combines macro-environmental and population analysis, involving molecular and microenvironmental analysis.
In addition, the goal of molecular pathological epidemiology is to explore the interrelationships between exogenous and endogenous factors, molecular markers, and progression of malignancy. More importantly, the study of molecular pathological epidemiology can cover all human diseases. Thus, molecular pathological epidemiological studies can provide insights into the pathogenesis of disease by confirming specific mechanisms during disease development and progression.
7. Evidence for the application of molecular pathological epidemiology in colorectal cancer research
It has been well established that traditional epidemiological investigation shows that many factors, such as lifestyle, diet and environmental exposure, can be positively or negatively related to risk. disease chance. However, it remains unclear how these exposures affect the pathogenesis. Previous studies have confirmed that these factors can influence the pathogenic process by alteration. As the local tissue environment and epigenetic inheritance play an important role in the cellular response to changes in the microenvironment. There is increasing evidence supporting the application of molecular pathological epidemiology in colorectal cancer research to identify possible etiological factors. However, little is known about the molecular pathological epidemiology study of ulcerative colitis. It is considered a heterogeneous disease in which smoking, alcohol, diet, obesity, microbiome, inflammation, immunity, germline genetic variations and interactions between genes are cause of the progression of ulcerative colitis.
Therefore, molecular pathological epidemiology can be useful to investigate factors that are related to molecular pathology, immunology, and clinical outcomes. Although molecular pathological epidemiology research has many advantages, challenges should also be considered.
8. Diagnostic challenges
Mainly reported challenges in molecular pathological epidemiology research include selected sample size, severe validation requirements of molecular tests, research discovery, lack of multidisciplinary experts , international forums, as well as standardization strategies. Furthermore, molecular pathological epidemiological studies face the problem of challenging different hypotheses. Therefore, it is required to form a priori hypotheses on the basis of early discovery or possible biological mechanisms. Furthermore, molecular pathological epidemiology may also create more opportunities for false findings. When considering the pathogenesis of ulcerative colitis, molecular pathological epidemiology modeling could be a promising direction and improve the prediction of response to pharmacological, dietary and lifestyle interventions. survival for ulcerative colitis, along with the pathogenesis and treatment of mucosal lesions of the upper gastrointestinal tract in patients with ulcerative colitis.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Sun Y, Zhang Z, Zheng CQ, Sang LX. Mucosal lesions of the upper gastrointestinal tract in patients with ulcerative colitis: A review. World J Gastroenterol 2021; 27(22): 2963-2978 [DOI: 10.3748/wjg.v27.i22.2963]