This is an automatically translated article.
The article is professionally consulted by Master, Doctor Phan Ngoc Toan - Emergency Medicine Doctor - Emergency Department - Vinmec Danang International Hospital. The doctor has a lot of experience in the treatment of Resuscitation - Emergency.1. Overview
Subcutaneous emphysema (TKDD) is the generation or penetration of air into the subcutaneous layer of the skin. The skin is composed of the epidermis and dermis, with subcutaneous tissue beneath the dermis. However, the development of a subcutaneous emphysema may indicate that the air is occupying another area deeper in the body that is not visible to the naked eye.Pneumothorax into other body cavities and spaces can cause pneumomediastinum, pneumoperitoneum, and pneumothorax. Air moves from these areas according to the differential pressure between the alveolar lumen and the perivascular interstitium, spreading to the head, neck, thorax, and abdomen by connecting the anatomical planes and the omentum. Air will accumulate in areas of the skin that have the least tension until the pressure is increased enough to split along other planes, causing subcutaneous spread and possibly respiratory and cardiovascular collapse.

Mechanistically, air or gas penetrates into the dermis leading to subcutaneous emphysema. The skin from the fascia, mediastinum, and retroperitoneal space are connected by fascialplanes and air is allowed to follow this same plane and then move from one compartment to another.
Air can follow perivascular sheaths, into the mediastinum and from there into subcutaneous tissue, if the lung is punctured (whether parietal or visceral). Similarly, excessive pressure in the lungs may have ruptured the alveoli during barotrauma, and air rushed below the visceral pleura, up to the hilum, along the trachea, and into the neck.
In thoracic trauma, the presence of subcutaneous pneumothorax usually indicates a severe thoracic injury involving the air-filled structures in the thorax.

2. Cause
ASD can be surgical, traumatic, infectious, or spontaneous. Trauma to the thoracic cavity, sinuses, facial bones, barotrauma, bowel perforation, or rupture of a pneumococcal cyst are some of the more common causes.Medical treatment causes such as ventilator-related failure, Valsalva maneuvers that increase thoracic pressure, and airway trauma. Air can enter the subcutaneous compartments due to minor mucosal injury in the trachea or pharynx during intubation due to trauma, excessive endotracheal tube (ET) effusion, or increased airway pressure. breathing when the glottis is closed. Esophageal injury during nasogastric tube placement can also create openings to the airways.
Air can enter the subcutaneous tissue through the soft tissues of the neck during tracheostomy, through the chest wall during shoulder arthroscopy, through the extremities due to occupational accidents, through the intestines or perforation of the esophagus. without pulmonary trauma, either through thoracotomy or during central venous access procedures, or percutaneous or transbronchial lung biopsies.
TKDD has also been observed after air release during laparoscopy and through female genital tract during pelvic examination, douching, postpartum exercise...
3. Mechanism
The development of subcutaneous emphysema is thought to be due to the following mechanisms:Lesions of the parietal pleura allow air to enter the pleura and subcutaneous tissue Air from the alveoli spreads into the endothelial cortex and hilum into the lungs. fascia (parietal pleura) in the thoracic cavity. Mediastinal air spread between cervical viscera and other connective tissue planes Air of external origin Localized gas formation due to infection, particularly necrosis

4. Symptoms
The most common symptom is a crackling/crackling sound when palpating the suspected schizophrenia, depending on the patient's condition, there may be pain, moving air bubbles, or bulging deformities in the abdomen, chest, neck, and face. ...Eyelid edema that affects vision and voice changes or wheezing due to pressure on the vocal cords may also be present
In patients with widespread neuropathy, hematologic effects may occur. mechanical or respiratory, which is why it is important to investigate the cause of subcutaneous emphysema in each patient.
5. Diagnostic Imaging
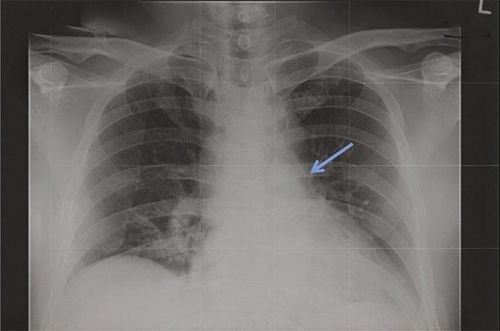
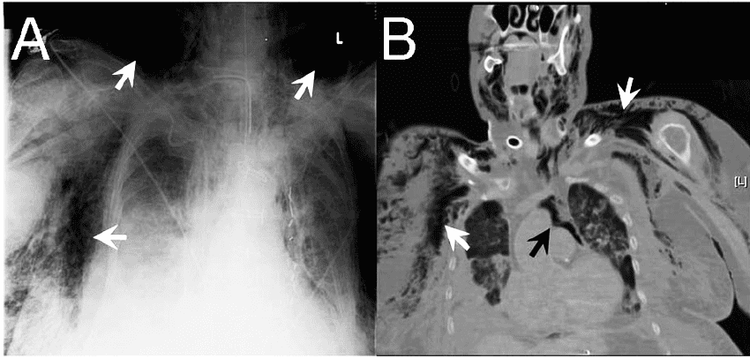
On radiographs, there are discontinuous (enhanced) areas, often with fine ridges on the outer border of the thorax and abdominal wall. On chest x-ray, air bands along the pectoralis major muscle can be seen, resembling a ginkgo leaf.Computed tomography (CT Scan) will show black sacs in the subcutaneous layer that are indicative of gas. CT may be sensitive enough to identify the source of the injury causing the ASD that is not visible on lateral or anteroposterior radiographs. If neck or facial schizophrenia occurs during intubation, laryngoscopy should be performed prior to extubation to assess for impending airway injury or pneumothorax. In addition, if intubation-induced airway damage is suspected, bronchoscopy can help locate the tracheal lesion.
Ultrasound, although air acts as an acoustic barrier when using ultrasound, neurodegenerative disorders can present with scattered hyperechoic. By placing the ultrasound probe over an area of skin without pneumothorax, it is possible to diagnose a pneumothorax due to the absence of “sliding lung” and “A line” signs with a sensitivity of 95%
6. Treatment
Treatment of the underlying cause or predisposing factor should be considered first as it often leads to gradual resolution of the ASD. For mild cases that do not cause significant patient discomfort, only observation is needed. In patients who experience persistent discomfort or require rapid resolution, high-concentration oxygen is a common treatment, allowing nitrogen clearance and diffusion of air particles in patients with concomitant pneumothorax. and/or pneumomediastinum disease.During intubation, trauma can occur to the posterior wall of the trachea, causing a mucosal tear. A tracheostomy may be required to bypass the tear and prevent further subcutaneous emphysema or other complications. In the presence of mucosal tear, empiric broad-spectrum antibiotics may also be beneficial to prevent the development of mediastinitis. For mechanically ventilated patients, reducing VT, PEEP, and minimizing bronchospasm and air trapping can prevent progressive pneumothorax and promote resorption...
In patients with subcutaneous emphysema spread, it has been reported that bilateral 2cm incisions can reduce further spread of subcutaneous gas. In one case report, a patient with extensive TKDD after thoracotomy was successfully treated with a low-pressure suction tube placed shallowly under the skin to the thoracic fascia. Most specialists reserve invasive therapy for cases of increased airway compression or cardiovascular damage.
7. Differential diagnosis
In a limited number of case reports, TKDD has been confused with an allergic reaction and angioedema after the patient presented with difficulty breathing and facial swelling. Physical examination can help distinguish between the two because TKDD is not present in the lips. While GERD does not spread and is not life-threatening, it can be a clue to other life-threatening conditions that need to be checked and ruled out including esophageal rupture, pneumothorax, tracheal perforation. /intestinal/diaphragm and necrotic infection. It is important that, after intubation, not only consider barotrauma due to alveolar injury as the source of ASD but also examine tracheal tears caused by intubation.8. Prognosis
Most subcutaneous emphysema is not fatal and is self-limited. Even in the case of positive pressure mechanical ventilation, TKDD is considered benign and does not require ventilation adjustment. However, in cases where the gas expands rapidly and heavily, it can be life-threatening. Massive dyskinesia can cause compartment syndrome, preventing chest wall expansion, tracheal compression, and tissue necrosis. Among these dreaded complications, if left untreated, respiratory and cardiovascular depression can occur. Gas volume expansion will also be accelerated with the use of nitrous oxide and positive pressure ventilation, rapidly worsening prognosis and possibly contributing to increased morbidity and mortality.9. Complications
Widespread pneumothorax in the subcutaneous tissues can prevent thoracic expansion, make it difficult to achieve adequate ventilation, lead to desaturation, respiratory failure, and threat of cardiac arrest. Air entering the neck can make it difficult to swallow and compress or close the airway. On ventilatory support, if an adequate volume of ventilation cannot be achieved, peak pressure can result and cause pressure injury or widespread pneumothorax. If LVEF impedes thoracic outlet, it can prevent adequate airflow, reduce cardiac preload, and lead to poor cerebral perfusion. Gynecomastia can disrupt the delicate blood vessels supplying these areas, causing skin necrosis. In patients with pacemakers, it can cause device dysfunction due to air retention in the pulse generator.Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.