This is an automatically translated article.
Bovine spongiform encephalopathy, also known as mad cow disease (English name is bovine spongiform encephalopathy, abbreviated BSE). The disease originated in England in the 1980s, lasted into the 1990s with more than 100,000 children affected. The disease is dangerous to humans, has a high risk of death, and cannot be treated.
1. The concept of spongiform encephalopathy
Bovine spongiform encephalopathy is a serious condition in which the brain and spinal cord (central nervous system) in cows is gradually destroyed. Causes them to have abnormal expressions, behavior, difficulty in movement and weight loss. Spongiform encephalopathy or mad cow disease has the ability to spread to humans, causing degenerative disorders of nerve cells in the brain leading to memory loss and death.
2. Causes of spongiform encephalopathy
The cause of this disease is thought to be infection with a toxic protein, called a prion, so the disease is also known as prion disease. Prion diseases are caused by the incorrect helix structure of a normal cell surface brain protein called prion cytoskeletal protein (PrPC). Once in the body, these toxic proteins affect other normal proteins, making them new prions. Just like that, they will grow in the body more and more. Thereby, causing changes in biological reactions in the body.
Bệnh não xốp do một loại protein độc gây ra
3. Manifestations of spongiform encephalopathy
Manifestations of people with spongiform encephalopathy are typical, rapidly progressing, mentally impaired and occur only for a few months. The most commonly seen signs include:
Change in personality (patient is often irritable, angry...) Anxiety Or sadness, depression Memory loss, even memory loss ( poor memory ability, forgetfulness, forgetting at the same time) Mental confusion Reduced vision or blindness Sleep disturbances (insomnia, sleep or tossing) Difficulty speaking Difficulty swallowing Movement difficulties (walking difficulties, jerking hands and feet). Spongiform encephalopathy progresses very quickly, the symptoms get worse, most of the patients are usually comatose. People with severe spongiform encephalopathy also lead to heart failure, respiratory failure, pneumonia, even infection, and then death. Death is usually noted one year after the onset of disease.
4. How is spongiform encephalopathy transmitted?
Although it is a dangerous disease, spongiform encephalopathy is very difficult to transmit. The disease is not transmitted by coughing, sneezing, direct contact or sexual contact. Accordingly, spongiform encephalopathy is transmitted through the following three ways:
4.1. Random transmission
This is the most common form, most cases of prion disease do not identify where the infection comes from, how it is transmitted. Therefore, also known as disseminated prion disease.
4.2. Spongiform encephalopathy is hereditary
5- 15% of cases run in families. The gene mutations that cause prion disease are inherited through the autosomal dominant gene 20. If one parent has spongiform encephalopathy, there is a high chance that the child will also have it. So this is also known as familial mad cow disease.

Bệnh não xốp có tính chất di truyền
4.3. Due to contagion
This is the rarest form and can be transmitted as follows:
From person to person: due to unsatisfactory medical procedures for organ and tissue transplantation, such as cornea or transplant. skin graft. Due to the unusual use of surgical instruments contaminated with prions because standard sterilization methods do not destroy them. Or, more rarely, in blood transfusions. Animal to human: Through eating beef contaminated with mad cow disease (in vCJD). But according to research, milk and dairy products do not pose a risk of transmitting BSE to humans, including cows that have the disease.
5. People at high risk for spongiform encephalopathy
Worldwide, it is estimated that one person in one million people gets mad cow disease each year. Those at high risk are often related to:
Genetics: If there are close relatives like parents or grandparents infected, the next generation will also get the disease. Exposure to Contaminated Tissue: People who have received human pituitary-derived growth hormone or who have had a brain-enveloping tissue transplant are at increased risk of developing this condition as a result of treatment. Age factor: the disease is common in elderly people, usually around 60 years old. Family-transmitted mad cow disease manifests earlier, most commonly in young people in their late 20s. The risk of spongiform encephalopathy is difficult to determine after eating contaminated beef. In countries around the world, where public health measures are effectively implemented, the incidence of the disease is almost non-existent.

Người cao tuổi là đối tượng dễ có nguy cơ mắc bệnh não xốp
6. Measures to prevent spongiform encephalopathy
Transmissible spongiform encephalopathy can come from a variety of origins that cannot be identified. So to effectively prevent disease, you can rely on some of the following methods:
Control and manage diseased animals. Changing the way of raising and destroying sick cows. Limit the import of livestock from countries and regions where BSE is common. Animal feed should be strictly managed. Monitor and monitor livestock health Limit the use of products from infected cows, especially parts containing a lot of prions such as the brain, spinal cord, and intestines Practice good hospital infection control Minimize risk human-to-human transmission through infusion, organ transplantation by carefully examining the donor Surgical instruments should only be used once on a sick person.
7. Diagnostic methods for spongiform encephalopathy
Brain biopsy or postmortem examination of brain tissue (autopsy) is the only method of diagnosing spongiform encephalopathy. But doctors can also make an accurate diagnosis based on your medical history, neurological examination, and diagnostic tests.
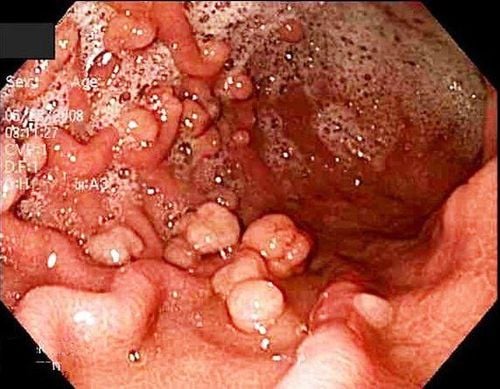
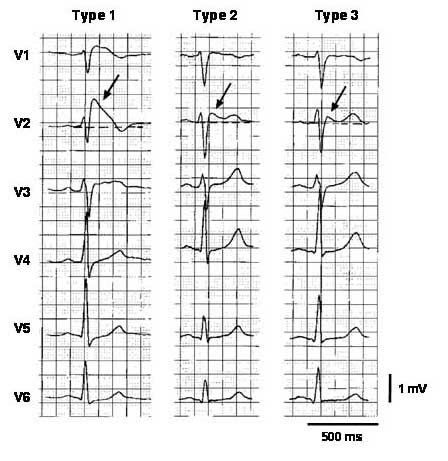
In addition, based on the clinical manifestations of the disease, doctors will use the following test methods to detect mad cow disease:
Electroencephalogram (EEG): place electrodes on the patient's scalp and then measure the electrical activity of the brain. If the patient has BSE, an abnormal and characteristic brain wave image will be produced. MRI or magnetic resonance imaging is an imaging technique that uses a magnetic field and radio waves to create cross-sectional images of the patient's head and body. This method is very useful in diagnosing brain disorders because the images of white and gray matter of the brain are very clear making it easier for doctors to see; Spinal fluid aspiration: In this test, the doctor uses a needle to aspirate a small amount of cerebrospinal fluid and examine it. If a particular protein is detected in the cerebrospinal fluid, this is a sign that the patient may have mad cow disease.

Chụp MRI cho phép chẩn đoán bệnh não xốp
8. Measures to treat spongiform encephalopathy
Currently, spongiform encephalopathy still has no treatment. For this reason, doctors often use pain relief and symptom relief to help patients feel less uncomfortable and more comfortable.
Although it is a rare and uncommon disease, mad cow disease is very serious and cannot be cured. People with spongiform encephalopathy often progress rapidly and have symptoms that may resemble Alzheimer's disease. Therefore, patients often subjectively make the disease worse and eventually lead to death. Mad cow disease is very dangerous, so it is necessary to take good precautions to avoid transmission, thereby reducing the incidence of the disease.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.