This is an automatically translated article.
The article was professionally consulted by Specialist Doctor II Nguyen Binh - Department of General Surgery - Vinmec Ha Long International Hospital. Doctor Nguyen Binh has more than 20 years of experience in the field of anesthesia and resuscitation.1. What is brain death?
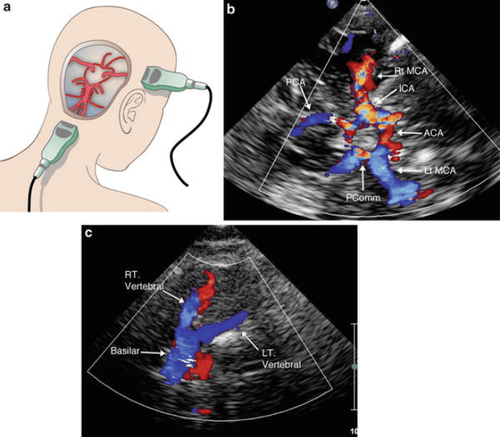
Brain death is the complete loss of function of the brain and brain stem. The brainstem is a structure connecting the two hemispheres of the brain and the spinal cord, which transmits nerve signals from the brain to the periphery through the spinal cord. Besides, the brain stem is also the place to regulate and control important life activities of the body, including respiration, circulation and temperature regulation. A patient was diagnosed with brain death when the functional activities of the brain, heart, and lungs were completely stopped. Clinical manifestations that doctors and family members can observe such as heart beat, warm and pink extremities, soft body are thanks to medical support devices. Unlike clinical death, brain death is a state of permanent and irreversible damage.In clinical practice, there are many patients admitted to the hospital in the context of a deep coma, EEG tests do not detect normal brain waves, also known as flat electroencephalograms, but other organ systems are still present. can function on its own as the heart beats, urine is also produced. These cases were understood to include incomplete death or decerebral extensor.
The cause of death is quite diverse, different in each patient. Some patients have only one fatal brain lesion, while others have multiple causes. The most common causes of brain death include traumatic brain injury, subarachnoid hemorrhage, intraparenchymal bleeding, meningitis, and meningeal abscess. When intracranial pressure rises above mean blood pressure, blood cannot be pumped from the heart to the brain. At that time, the brain cells lack oxygen nourishment, become edematous and continue to increase intracranial pressure, creating a complex pathological circle.

2. Diagnostic criteria for brain death
Concluding a brain dead patient is a legal job and requires high accuracy. Brain death was determined through the combined use of a variety of information including clinical symptoms, clinical trials, laboratory methods, and time to brain death.Clinical criteria for the diagnosis of brain death include the following symptoms:
Glasgow score : 3 as evidence of falling into a deep coma Loss of light reflexes Diameter of fixed dilated pupils about 4mm both eyes The corneal reflex to protect the eye disappears Cough reflex when there is a stimulus such as sputum suction is gone. The head-eye reflex is gone. The vestibular eye reflex is gone. When the ventilator is removed, the patient is not able to breathe on his own. After a brain death condition is suspected, the doctor will perform other clinical tests to confirm the diagnosis including:
Cough test: while performing sputum aspiration through the endotracheal tube, Stimulation was performed at the bifurcation site of the main bronchus, but the cough reflex did not appear. Check head-eye reflex: tilt the patient's head to one side but the eyeball does not move to the opposite direction. Vestibular eye reflex test: perform cold water injection into both ears but the eyes do not respond by glancing toward the ear with the water pump. The vestibular eye reflex is performed when the head reflex test is inconclusive. Apnea test: put the patient on a ventilator for about 10 minutes with 100% oxygen content, then remove the ventilator and let the patient breathe through the endotracheal tube for 10 minutes. The apnea test is positive when the patient is unable to return to breathing on his own. Paraclinical criteria to help diagnose brain death include:
EEG: conduct EEG measurement to show flat brain waves. normal brain waves were not observed.
Determining a brain death is a complex legal process. The Ministry of Health stipulates that the team to diagnose brain death must include 3 doctors who meet the prescribed conditions. Repeat tests to diagnose brain death at 6 and 12 hours from the first diagnosis.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.