This is an automatically translated article.
Article by Specialist Doctor I Nguyen Cong Hoa - ICU Doctor - Intensive Care Department - Vinmec Times City International General Hospital.
Because ultrasound cannot pass through the thick bone plate of the skull, but certain windows allow ultrasound waves to pass through. Taking advantage of these windows, transcranial doppler ultrasound machine with low frequency transducer, 2 MHz frequency ultrasound probe was used to investigate the cerebrovascular system.
1. What is transcranial doppler ultrasound?
Transcranial doppler ultrasound is a noninvasive, non-ionizing, inexpensive, portable and safe technique that uses a pulsed Doppler probe to evaluate blood flow in the brain.
The advantages of transcranial Doppler ultrasound are:
Assess the transport function of the vessels. Non-invasive, no harm to health. Low cost. Can be done many times. Performed at bed. Disadvantages of transcranial Doppler ultrasound are:
Cannot evaluate the morphology of vessels and organization.
2. Transducer types of transcranial doppler ultrasound machine
Continuity transducer:
Transducer with 2 crystals Continuity of sound waves Continuity of sound waves The advantage of the continuous transducer of transcranial doppler ultrasound is that it can measure very high velocities. However, the disadvantage is that the speed is not recorded at one point, but the average speed of many points the beam meets along the way.
For example, when sound waves pass through two adjacent blood vessels, the recorded speed is the average speed of the two blood vessels.
Pulse probe:
The probe has a crystal that both transmits and receives. The wave propagates in sequence of pulses. Only the feedback pulse at the sampling site is analyzed. The advantage of the transcranial doppler pulse probe is the determination of the location of the flow. The disadvantage is that the high velocity flow cannot be measured, the time T for the outgoing and returning pulses determines the shortest time interval between two pulses, the repetition frequency of the PRF pulses cannot be greater than 1/ T.
3. Principle of ultrasonic shaping
The time it takes for the sound wave to travel back and forth indicates the depth of the feedback surface: d = c * t/2 (c: speed of sound propagation in the body; t: time it takes for the sound wave to travel back and forth; d: depth feedback side).
The magnitude and amplitude of the reflected wave depends on the amplitude, angle of incidence, environmental acoustic impedance, and size of the feedback surface. The transducer converts the echo into an electrical signal.
Echo wave:
Magnitude, speed information. Location information. This information is processed and expressed into audio and visual signals.
Display modes:
A mode: The signal shows spikes, the height is the magnitude, the position is the distance from the probe to the feedback surface; This type of representation is used in measurement because of its high accuracy. B mode: Signal represents light dots, amplitude brightness, dot position is the distance from the transducer to the feedback surface. M mode: Displays flow strength and direction over a length of about 6cm or more; the advantage of displaying all possible flow signals at a time on the same screen. Transcranial doppler signal received is shown through:
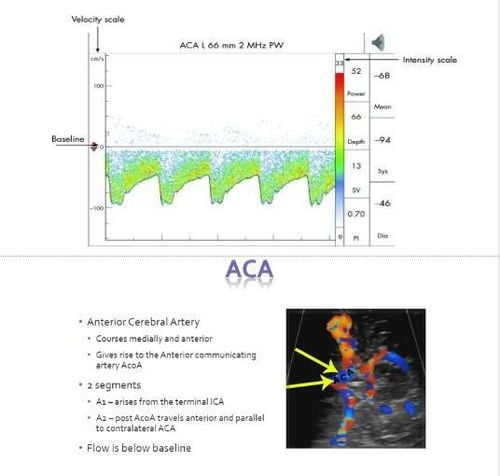
Sound: Doppler frequency, amplifier, speaker, ear. Timbre and loudness due to different frequencies and amplitudes. Smooth, continuous flow. The flow is more compact than the artery. However, it is subjective and qualitative. Doppler spectrum: A doppler frequency image is made of moving blood cells in an area of the vessel lumen examined over time. Analyze a complex signal into discrete frequencies of corresponding amplitude and time progression. Spectral analysis is performed using Fourier series analysis algorithm (F.F.T - Fast Fourier Transform). Expressed by velocity type: Peak Systolic Velocity (PSV); end-diastolic velocity (EDV); average velocity (MFV). Doppler spectral information: Peak Systolic Velocity (PSV) has a rate corresponding to the systolic peak; end-diastolic velocity (EDV) has a rate corresponding to end-diastolic; average velocity (MFV); flow direction towards red probe, above baseline and vice versa; signal intensity depends on the number of red blood cells at the same rate, the darker the more cells with the same speed through the survey site; scale (scale) speed, too small aliasing effect, too large error; increasing power does not increase noise. A diagram of Bernoulli's principle showing that when liquid flows from a pipe or vessel of larger diameter to a smaller diameter, the velocity of the flow increases and the pressure decreases to allow the same volume of liquid to pass. through a narrower area. Therefore, the velocity of blood flowing through areas of narrowing secondary to vasospasm in the setting of subarachnoid hemorrhage is expected to be higher than that of blood flowing through adjacent vessels.
4. Transcranial doppler ultrasound windows
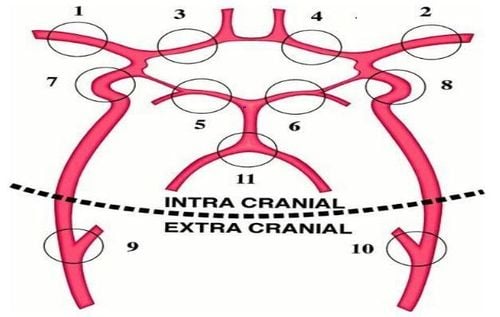
Willis polygon
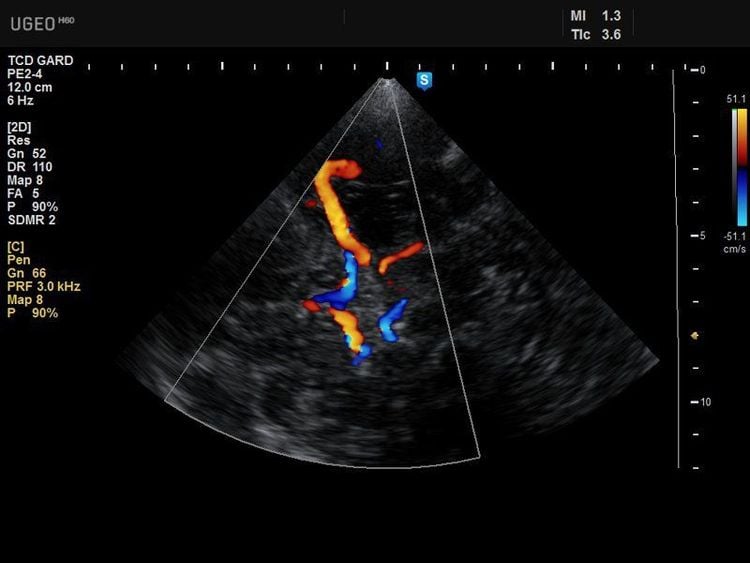
Middle cerebral artery. The middle cerebral artery (MCA) is identified through the temporal window, with normal flow direction towards the transducer, so the spectrum is red, about 30–60 mm from the skull surface. The fundamental wave is above the baseline, the Yang wave.
A typical transcranial Doppler spectrum with velocity and magnitude scales on the left and right axes respectively. Waves above the baseline reflect flow toward the transducer (normal middle cerebral artery (MCA) fistula at 50 mm depth - transcerebral window).
Anterior cerebral artery. ACA is performed at the temporal window at a depth of 65–80 mm with the transducer facing anteriorly and upwards. The figure below is the normal anterior cerebral artery (ACA) probe side probe at the temporal window at 66mm depth with downstream flow distal to the transducer so blue spectrum, subbasal baseline waveform, waveform minus.
Posterior cerebral artery. The posterior cerebral artery (PCA) is probed at the temporal window at a depth of 55-70 mm with the probe facing posteriorly and downward. PCA is divided into two segments: P1 and P2. In the P1 segment, the flow is directed towards the transducer, so there is a red spectrum and a wave above the baseline (positive wave). The segment P2 goes away from the transducer so there is a blue spectrum and a wave below the baseline (Acoustic wave).
At the eye window we have to use low energy level of ultrasound, to protect the eyes, tegaderm patch can be used on the eye to avoid infection when applying gel for transcranial doppler ultrasound. At the eye window we will examine the ophthalmic artery, the intracranial ICA, specifically the C4 and C2 segments.
Ocular artery depth 40-60mm, flow towards the transducer, red spectrum, positive wave, average velocity 16-24cm/sec. Occipital window (picture below). We will examine 2 vertebral arteries and basilar arteries.
The basilar artery (BA) is examined at a depth of 60-90mm, the flow direction is far away from the transducer, blue spectrum, sound waves.
Two vertebral arteries surveyed at depth of 40-80mm, flow direction away from transducer, blue spectrum, sound wave.
5. Clinical application of transcranial doppler ultrasound machine
Subarachnoid haemorrhage and cerebrovascular vasospasm Cerebral vasospasm (VSP) occurs in two-thirds of patients with subarachnoid hemorrhage (SAH) from ruptured aneurysm with one-half being symptomatic.
There is a significant direct correlation between the severity of cerebral vasospasm in subarachnoid hemorrhage and the flow velocity in most cerebral arteries, despite anatomical factors and sonographic techniques. weakening the association of ICA and ACA.
DSA can be considered the gold standard in this case. However, DSA brain angiography is invasive, expensive, not always immediately available, and not without risks. Transcranial Doppler (TCD) has been suggested to diagnose cerebral vasospasm. The diagnosis of spasm using a TCD device is based on the hemodynamic principle that the velocity of blood flow in an artery is inversely related to the lumen area of that artery.
In theory, TCD can be used as a relatively simple screening method for cerebral vasospasm, and some researchers have advocated replacing angiography with TCD.
Today TCD is performed by many stroke and neurosurgery units.
Intracranial stenosis Intracranial atherosclerosis is a significant risk factor for ischemic stroke and transient ischemic attacks (TIAs), accounting for ~10% of such events . TCD can be used to detect carotid stenosis, proximal MCA, ACA, PCA, and intracranial vertebral arteries.
Because of the greater deformity and anatomy of the vessels in the posterior circulation, the sensitivity, specificity, positive predictive value, and negative predictive value of TCD are generally higher than in the anterior circulation.
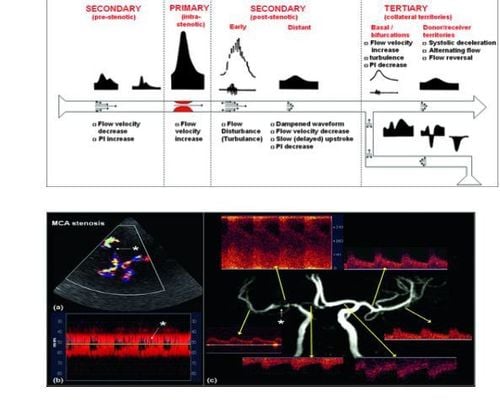
Midbrain artery stenosis (MCA) image (white star) on transcranial 2D (TCDI) (a) and M-Mode (b). Flow turbulence can be easily seen on both 2D TCDI and M-Mode modes. Spectral changes are shown (c). There was a significant increase in flow velocity in the stenosis (PSV 300; Vmean: 220; EDV: 180cm/s) and decrease in the posterior stenosis (PSV: 60, Vmean: 40; EDV: 30cm/s and delay). stroke up 0.25 seconds).
Significant negative predictive value (86–94% for MCA and 88% for VA/BA).
The relatively low positive predictive value (36–73% for MCA and high 93% for VA/BA) suggests that TCD is a reliable tool to rule out the presence of intracranial stenosis. Higher thresholds such as PSV = 300 cm/s and Vmean = 200 cm/s may present with intracranial stenosis (> 80%).
Acute ischemic stroke
TCD is particularly useful in acute ischemic stroke, where TCD studies can be used to monitor pre and post fibrinolysis in patients cerebrovascular occlusion due to thrombosis. TCD can detect thrombosis causing acute MCA occlusion with high sensitivity (>90%), TCD can also detect occlusion in the siphon of the internal carotid, vertebral and basilar arteries with reasonable sensitivity. (70 to 90%) and positive predictive value and high specificity and negative predictive value (>90%).
Sickle cell disease
Children with sickle cell disease (SCD) have chronic hemolysis resulting in low hemoglobin. Chronic anemia and hypoxia trigger angiogenesis and neovascularization. In addition, the interaction of sickle cells with the endothelium causes inflammation and narrowing of the intracranial arteries. The damaged vascular system makes these children susceptible to ischemic and hemorrhagic infarction. An increase in V mean (mean) V 200 cm/sec, in the ICA or MCA arteries as detected by TCD has been shown to be associated with an increased risk of ischemic stroke in children. this.
In the STOP trial (Trial for stroke prevention in sickle cell anemia). A primary prevention approach that includes close TCD monitoring and frequent blood transfusions for high-flow velocities of MCAs on TCD has become a standard of care for children with sickle cell anemia. . Since early TCD screening combined with blood transfusion prophylaxis appears to reduce stroke rates in children with sickle cell anemia, TCD assessment should now be a routine component of preventive care for children with sickle cell anemia. these children.
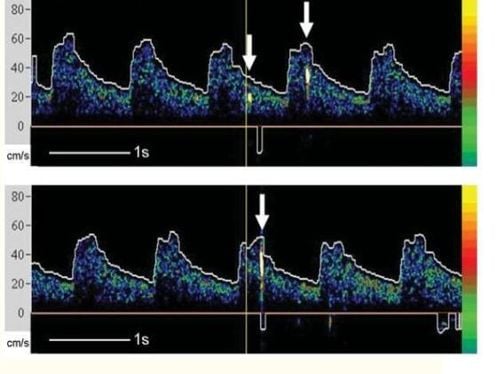
Microemboli Detection
TCD is the only medical device that can detect circulating brain emboli microphones, both solid and gas, in real time. Detection of microemboli TCD is based on backscattering of ultrasound waves from emboli resulting in a high-intensity transient signal (HITS), higher backscattering of ultrasound from air embolism compared to solid emboli of similar size. is, in turn, higher than the backscatter observed from red blood cells in normal flow. High-intensity transient signals (HITS), seen with embolization, have been detected by TCD in patients with carotid stenosis, myocardial infarction, atrial fibrillation, and mechanical heart valves.
Increased intracranial pressure and cerebral circulatory arrest TCD provides an indirect estimate of ICP and cerebral perfusion pressure (CPP). Decreased EDV and increased PI are the early sonographic changes observed with increased ICP. An increase in ICP and a further decrease in EDV is known as reversible (or biphasic) diastolic flow.
PI increases exponentially after flow reversal, and PSV begins to decrease depending on residual cerebral perfusion pressure. It is important to note that the absolute values of PI are not very useful for estimating ICP.
However, modeling waveform changes over time in a particular patient has the benefit of predicting corresponding ICP changes. In patients with increased intracranial pressure and midline changes, color Doppler/B-mode imaging provides direct structural information such as the location of the third ventricles and optic nerve sheath hypertrophy.
Continued elevation of ICP to too high can lead to complete cessation of flow through the cerebral microcirculation, termed cerebral circulatory arrest. This indicates a lack of cerebral perfusion and, if prolonged, eventually leads to brain death. In subjects without detectable intracranial flow, TCD is up to 95% likely to confirm brain death.
Doctor Nguyen Cong Hoa has more than 16 years of experience in the field of Emergency Resuscitation, especially with deep expertise in emergency and resuscitation of critically ill patients with neurological, cardiovascular, respiratory, digestive, nephrology, pediatrics.
Currently, Doctor Nguyen Cong Hoa is holding the position of Intensive Care Doctor at the Intensive Care Unit - Vinmec Times City International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.