This is an automatically translated article.
The article is expertly consulted by MSc.BSCKII Phan Thi Minh Huong - Gastroenterologist, Vinmec Danang International General Hospital.Liver function tests help determine the health of the liver by measuring the levels of proteins, liver enzymes, and bilirubin in the blood. The liver performs many important functions in the body, so regular liver function checks are essential. Therefore we should find out what the test indicators include and how to read the results, let's follow the article below.
1. What is a liver function test?
Liver function tests help your doctor check your liver's function and detect liver damage. These blood tests measure the levels of proteins and enzymes in your blood.Liver function tests are usually recommended in the following situations:
Check for damage from liver infections, such as hepatitis B and hepatitis C Watch for side effects of certain medications known to affect liver History of liver disease, to monitor the disease and how to treat it especially effectively Patients with symptoms of liver disorders Patients with medical conditions such as high triglycerides, diabetes, high blood pressure or anemia Heavy drinking Gallbladder disease
Trắc nghiệm: Làm thế nào để bảo vệ lá gan khỏe mạnh?
Làm test trắc nghiệm kiểm tra hiểu biết về gan có thể giúp bạn nhận thức rõ vai trò quan trọng của gan, từ đó có các biện pháp bảo vệ gan để phòng ngừa bệnh tật.2. Some common liver function tests
Some liver function tests are grouped as follows:The test group evaluates liver necrosis. The test group investigates the function of excretion and detoxification. General functional testing group.
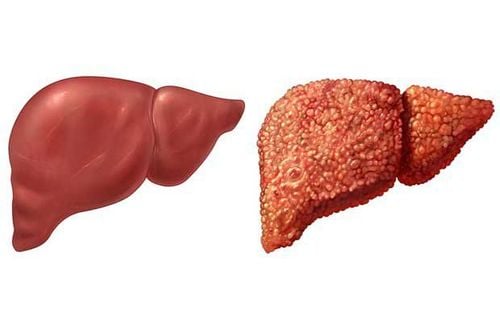
Các bệnh về gan khuyến khích xét nghiệm chức năng gan
2.1 The test group evaluates hepatocellular necrosis AST (Aspartate aminotransferase) is more present in cardiac muscle and skeletal muscle than in liver. In addition, AST is also present in the kidneys, brain, pancreas, lungs, white blood cells, and red blood cells. Normal AST < 40 UI/L. ALT (Alanine aminotransferase) is present mainly in the cytoplasm of hepatocytes, so ALT elevation is more sensitive and specific than AST in liver diseases. Normal ALT < 40 UI/L. Transaminases are elevated in most liver diseases but are not completely liver-specific because they are also elevated in other conditions such as myocardial infarction, skeletal muscle damage (myositis, muscular dystrophy), hyperthyroidism or hypothyroidism, celiac disease... In contrast, these enzymes may be artificially reduced in the presence of hyperuremia.
Elevated levels of transaminases are associated with some liver diseases as follows:
Elevated levels (> 3000 UI/L) can be seen in cases of hepatocellular necrosis such as acute or chronic viral hepatitis, liver damage due to drugs, toxins, prolonged vascular collapse Moderate increase (<300 UI/L) is seen in alcoholic hepatitis. Transaminase elevations were mainly AST but values were no more than 2-10 times the upper limit of normal. Mild elevations (<100 UI/L) may be seen in acute viral hepatitis, mild and focal or diffuse chronic liver disease (cirrhosis, chronic hepatitis, liver metastasis), biliary obstruction or fatty liver . For obstructive jaundice, especially common bile duct stones, ALT is usually < 500 UI/l. Lactate dehydrogenase (LDH) is a non-liver specific test because it is found in all tissues of the body (heart, muscles, bones, kidneys, red blood cells, platelets, lymph nodes). Elevated and transient LDH is seen in hepatocellular necrosis, liver shock. Persistent elevation of LDH with elevation of ALP suggests malignant infiltrative lesions of the liver. The ALT/LDH ratio can help distinguish acute viral hepatitis (ALT/LDH >1.5) from liver shock or acetaminophen toxicity (ALT/LDH <1.5). Ferritin: is a protein that stores iron in cells, keeping the task of regulating iron absorption in the digestive tract depending on the body's needs. Normally, ferritin in men is 100-300 mg/L, in women 50-200 mg/L. Decreased ferritin is seen in iron deficiency diet, iron deficiency anemia, fasting, bleeding bleeding, chronic hemolytic anemia, regular blood donors, hemodialysis. Increased ferritin is also seen in tissue iron overload, cancer (liver, lung, pancreas, breast, kidney), hematologic disease (Hodgkin's disease, acute leukemia), inflammatory and infectious syndrome, colloidosis. , alcohol poisoning, hemolytic anemia, thalassemia...
2.2 Test group to investigate the function of excretion and detoxification
Nhóm xét nghiệm khảo sát chức năng bài tiết và khử độc là xét nghiệm chức năng gan phổ biến
Increased bilirubin GT (usually <15 mg/dL): may be due to increased bilirubin production (hemolysis, ineffective erythropoiesis, reabsorption from hematomas) or decreased bilirubin capture by hepatocytes (Gilbert's syndrome).
Hyperbilirubinemia TT: associated with hepatobiliary disease, possibly due to decreased bilirubin excretion into the biliary tract or due to intrahepatic or extrahepatic cholestasis.
Bilirubinuria Only present in the form of bilirubin TT. When there is bilirubinuria, there is definitely a hepatobiliary problem. Bilirubinuria is detected quickly by dipstick. The results may be positive before clinically apparent jaundice, but by the time the patient's jaundice is gone, the bilirubinuria is negative before hypobilirubinemia.
Urobilinogen Is a metabolite of bilirubin in the intestine, is reabsorbed into the blood by the enterohepatic cycle and then also excreted in the urine. In the case of complete biliary obstruction, there will be no urobilinogen in the urine. Urobilinogen is increased in the urine in cases of hemolysis (increased production), gastrointestinal bleeding or liver disease. Normal urobilinogen 0.2 - 1.2 units (Watson method).
Alkaline phosphatase (alkaline phosphatase, ALP) ALP is an enzyme that hydrolyzes phosphate esters in alkaline medium (pH = 9). The primary origin of ALP is in the liver and bone. In the intestines, kidneys and placenta, it is less. Normal ALP 25 - 85 U/L or 1.4 - 4.5 Bodansky units.
Mild and moderate elevations in ALP (twice normal) may be seen in hepatitis, cirrhosis, metastases, or liver infiltration (leukemia, lymphoma, sarcoidosis). Elevated ALP (3-10 times normal) is usually due to intra or extrahepatic biliary obstruction.
5' Nucleotidase (5NT) This is a relatively liver-specific ALP that helps determine whether elevated ALP is liver- or bone-related or due to physiological conditions such as growing children or pregnant women. . An increase in 5NT was correlated with an increase in ALP. Normal 5NT 0.3 - 2.6 Bodansky units/dL
-g-glutamyl transferase , g-glutamyl transpeptidase (GGT, g-GT) Normal GGT
30 U/L in women and
50 U/L in male. The most common causes are chronic alcoholism, biliary obstruction, after taking some drugs that induce liver enzymes (acetaminophen, phenytoin) and some cases of nonalcoholic fatty liver. Also increased in renal failure, myocardial infarction, acute pancreatitis, diabetes mellitus, hyperthyroidism, chronic obstructive pulmonary disease.
Blood Ammonia (NH3) NH3 is produced from the normal metabolism of proteins in the body and by bacteria that live in the colon. The liver is responsible for detoxifying NH3 by converting it to urea for excretion by the kidneys.
Normal NH3 blood 5-69 mg/dL. NH3 is elevated in acute and chronic liver diseases. Blood NH3 is not a reliable test for the diagnosis of hepatic encephalopathy. NH3 can return to normal about 48 - 72 hours before there is an improvement in neurological status.
2.3 Integrated functional testing team
The majority of plasma proteins are synthesized from the liver.
Serum albumin The liver is the only site to synthesize albumin for the body. Albumin maintains intravascular oncotic pressure and is a carrier of substances in the blood, especially drugs. Normal albumin 35 -55 g/L. Blood albumin levels decrease only in chronic liver disease (cirrhosis) or when liver damage is very severe. In patients with cirrhosis and ascites, the amount of albumin decreases due to leakage into the ascites. Also seen in malnutrition or abnormal loss of albumin through the urine (nephrotic syndrome) or through the digestive tract (chronic colitis).
Serum Globulin Produced from many different places in the body, including many proteins that transport substances in the blood and antibodies that participate in the humoral immune system. Normal globulin 20-35 g/L.
In cirrhosis, globulin is elevated. In addition, elevated patterns of globulin types may also suggest specific liver diseases, eg, elevated IgG in autoimmune hepatitis, and elevated IgM in primary biliary cirrhosis.
Prothrombin time (PT) Is the time to convert prothrombin to thrombin in the presence of thromboplastin and Ca++ and coagulation factors. To normalize PT results, it is common to convert to INR (International Normalized Ratio). Normal INR = 0.8-1.2.
Prolonged PT is often a severe prognostic sign. Vitamin K deficiency due to prolonged biliary obstruction or fat malabsorption (fatty diarrhea, chronic pancreatitis) also prolongs PT, but with 10 mg of vitamin K injection, PT returns to at least 30% of normal within 24 hours. hours (Kohler test). Before surgery or a liver biopsy, blood clotting should be checked.

Xét nghiệm men gan cao theo định kỳ để bảo vệ sức khỏe tốt nhất
Evaluate the liver's ability to work through liver enzyme tests; Evaluation of bile function; vascular nutrition; Early screening for liver cancer; Perform tests such as Total blood cell analysis, blood clotting ability, screening for hepatitis B, C Assessment of liver and biliary status through ultrasound images and diseases that are at risk of affecting liver disease / liver disease. more severe liver disease In-depth analysis of parameters to evaluate hepatobiliary function through laboratory and subclinical tests; the risk of affecting the liver and early screening for hepatobiliary cancer
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference from source: Pasteur Institute