This is an automatically translated article.
Posted by Master, Doctor Nguyen Ngoc Phu - ICU Doctor - Intensive Care Department - Vinmec Times City International General Hospital
Tuberculosis of the spine is also known as tuberculosis of the spine. This is a form of tuberculosis caused by extrapulmonary bacteria and is the most common form of tuberculosis in the motility system. So at what age is the disease common and what is the most effective treatment today?
1. What is spinal tuberculosis?
Tuberculosis of the spine was described by author Percival Pott in 1779, so the disease is also known as Pott's disease. The most common in osteoarthritic tuberculosis (60-70%). It accounts for 10-35% of extrapulmonary TB cases and almost 2% of TB cases in general.
The disease usually affects the lower chest area and the upper lumbar region. Uncommon in the neck and upper thoracic region. The progression of spondylolisthesis usually begins with inflammation of the anterior aspect of the intervertebral disc joint, then spreads posteriorly to the anterior cruciate ligament, injuring adjacent vertebrae. When 2 adjacent vertebrae fuse together, inflammatory lesions will spread into the adjacent disc space.
The common age of spinal tuberculosis is currently 16-45 (62.4%). Injury is mainly in the disc and vertebral body (vertebral tuberculosis). Very rarely, tuberculous lesions of the posterior arc and spinous processes (posterior spinal tuberculosis). The common site of injury is the lower chest and upper lumbar region, the back 60-70%, the lumbar region 15-30%, the neck 5%, the sacrum very rarely.
About 70% of cases 2 vertebrae are affected and about 20% are affected by 3 or more vertebrae. The disease progresses into 3 stages, each stage has different symptoms and prognosis, the earlier the disease is diagnosed and properly treated, the better the prognosis.
The main cause of the disease is human tuberculosis bacteria, bovine tuberculosis bacteria may be encountered, very rarely atypical acid-resistant alcohol-resistant bacteria (NTM). Spinal tuberculosis usually appears 2-3 years after primary infection. Often seen after membranous TB and before visceral TB.
TB bacteria can spread from the primary infection to any bone or joint in the body. Normally, TB bacteria reach the joints mainly through the blood, rarely through the lymphatic route, possibly by the same approach as tuberculosis of the hip by spreading from the cold abscess of the lumbar muscle. The disease usually begins with inflammation of the disc joints and can spread to adjacent vertebral bodies. Damage to two adjacent vertebrae can lead to vertebral collapse.
2. At what age do you often get tuberculosis of the spine?
The age of previous disease was mostly young under 20 years old. Currently, tuberculosis of the spine is mainly found in adults, aged 16-45 years old. Young children who have not been vaccinated against TB with BCG vaccine, have had contact with the source of infection, especially the main and dangerous source of infection, with frequent and continuous contact.
The case has been and is being treated for primary TB, pulmonary TB or any other extrapulmonary TB. There may be some diseases of systemic nature such as: diabetes mellitus, peptic ulcer, partial gastrectomy. The body is immunocompromised, rickets, malnourished, infected with HIV/AIDS, severely exhausted.

Đối tượng chưa tiêm phòng lao với vắc-xin BCG có nguy cơ mắc lao cột sống khi tiếp xúc với nguồn lây
3. How is spinal tuberculosis diagnosed?
Diagnosis of spinal tuberculosis is based on clinical symptoms, subclinical, epidemiological and favorable factors. At the onset, the predominant symptom is pain (local or radicular pain).
Local pain: pain in the damaged spine, fixed pain, pain intensity more or less depending on each case, pain increases when moving, carrying, decreasing when resting. Pain increases gradually and pain relievers do not subside. Radial pain: due to irritating damage to several branches of the nerve root, usually bilateral, sometimes only one. If the injury is in the neck area, the pain usually radiates down the arm. If the lesion is in the back, the pain spreads downward along the femoral nerve or the sciatic nerve. Pain is persistent, prolonged, increasing. When examining the spine at the injury site, there is a stiff, not soft segment when doing movements (bends, backs, tilts, turns). Bilateral muscle mass is rigid, spine axis is straight and usually does not curve to one side. If you tap on the affected area, you will feel pain.
Patients may show systemic signs typical of tuberculosis (infection, chronic intoxication) such as: low-grade fever or moderate fever in the evening, prolonged, fatigue, poor sleep, thin weight loss. , pale skin, sweating theft.
When testing and scanning at this stage, we can see the following images of damage:
X-ray of the spine: very valuable for early diagnosis of spinal tuberculosis, but requires careful imaging. meticulous review and comment. It is necessary to capture the straight and inclined spine. The most common x-ray images are:
The disc is narrower than the superior and inferior vertebrae (most evident on lateral radiographs). The vertebral contour is blurred, the affected vertebra may be less intense than other vertebrae. Mild destruction of the vertebral body, especially the anterior and superior aspect. The soft tissue around the vertebrae is slightly darker than the surrounding area. In difficult cases, computed tomography or magnetic resonance imaging will show a vertebral body defect.
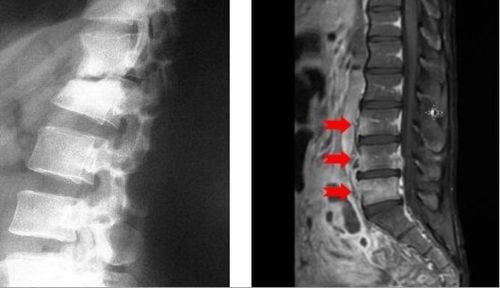
Xẹp nhẹ thân đốt sống do lao

Phản ứng mantoux: thường dương tính mạnh
Needle biopsy of the vertebrae, by surgery for histopathological and bacteriological diagnosis. Blood tests, lymphocytosis, elevated erythrocyte sedimentation rate.
At the full-blown stage, the lesion develops, the discs and vertebrae are destroyed much, forming a cold abscess around the injured area, showing signs of compression. This is an easy stage to diagnose, often months after the onset, and often difficult to treat. Patients usually have fixed pain in one area, constant pain, increasing. Radial pain is very pronounced. Limit movements such as bending, leaning, leaning, turning.
Examination of the patient will see that the vertebrae are backward, a vertebra protruding behind can be seen or palpated very clearly, in some cases, the damaged spine is crooked to one side. In addition, there may be signs of spinal cord compression: due to severe destruction of the spine and discs, displacement and compression on the spinal cord causes paralysis. Usually flaccid paralysis of the lower extremities, gradually increasing paralysis, accompanied by decreased sensation and circular muscle disturbances. Tuberculosis symptoms can be seen in other parts of the body: membranes, visceral organs, and peripheral nodes...
Signs of infection, chronic toxicity are becoming more and more obvious: frequent, continuous fever prolonged, increased height in the afternoon and evening, poor sleep, thin weight loss, pale skin.
Subclinical at this stage shows quite obvious lesions, including: On imaging: (X-ray, computed tomography or spinal magnetic resonance) The disc is narrow, almost lost. The vertebral body is heavily damaged, especially the anterior part, forming a wedge shape and falling posteriorly (tilt film). From the two joint surfaces of the two vertebrae above and below the lesion, an angle called Konstam-Blerovaky angle is drawn, this angle evaluates the hunchback of the spine.
May show cold abscess on straight radiograph
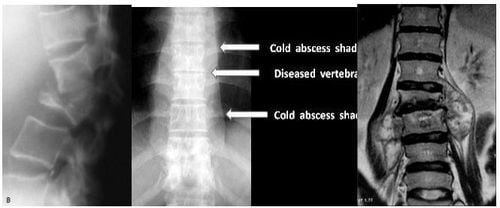
Xẹp thân đốt sống và khối Abscess lạnh cột sống do lao
Mantoux test positive. Aspiration, cold abscess pus to look for tuberculosis bacteria. Blood tests showed an elevated erythrocyte sedimentation rate and increased lymphocyte count.
When it comes to the end stage, if the patient is treated early and according to the principles, the systemic symptoms will improve, the lesions will stop progressing, the cold abscess will shrink, after 1-2 years the spine will stick, destroyed and regenerated gradually, the remaining sequelae are hunchback and limited mobility.
If not treated or the body is too exhausted, the disease can get worse, the damage spreads, spreads to other organs, compresses the marrow. The patient died of neurological complications and infection.
In fact, tuberculosis of the spine needs to be distinguished from other spinal diseases such as: spinal cancer (primary or secondary to metastases from other places), myeloma, ankylosing spondylitis , bacterial osteomyelitis, spina bifida, spondylolisthesis ...
4. How is spinal tuberculosis treated?
Currently, the treatment of spinal tuberculosis is still mainly medical, early treatment, right from the beginning. Combination of 4 to 5 anti-TB drugs in the attack phase, 2 to 3 drugs in the consolidation phase. Combination treatment with drugs to treat symptoms, prevent superinfection, protect the liver and improve physical condition.
Current treatment regimen for spinal tuberculosis is using a 12-month formula (2RHZE/10RHE). The patient will be treated for 2 months with 4 drugs Rifampicin (R), Isoniazid (H), Pyrazinamide (Z), Ethambutol (E). Previously, Streptomycin was often used, but due to its high toxicity on the kidneys, vestibule, and cochlea, it was replaced with Ethambutol. Children should not use Ethambutol in the consolidation phase.
Other treatment methods such as spinal immobilization waiting for stabilization (now rarely used), surgery (bursectomy, removal of cold abscess, removal of dead bone, spinal fixation, bio-cement pump). ..).
In order to serve well in the diagnosis and treatment of spinal tuberculosis, at present, Vinmec International General Hospital has a full range of modern X-ray machines, meeting international standards to perform examinations, Diagnosis of pathologies results in true, clear images and finding lesions and inflammation from the spine from which to have active treatment.
Besides, the examination process at the hospital is carried out by a team of highly qualified and experienced doctors, so customers can be assured of the medical quality at Vinmec.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.