This is an automatically translated article.
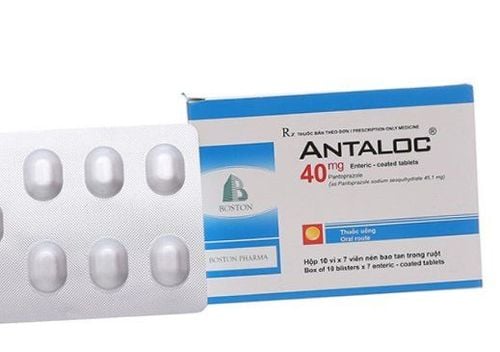
Panrixim medicine contains the main ingredients: Pantoprazole (as pantoprazole sodium sesquihydrate) 40mg, Clarithromycin 250mg and Tinidazole 500mg. Before using Panrixim, patients should consult a pharmacist or a specialist. The following is some information to help better understand what is Panrixim?
1. Uses and indications of Panrixim
Panrixim belongs to the group of gastrointestinal drugs, in the dosage form of film-coated tablets or enteric-coated tablets.
Pharmacodynamics:
The active ingredient Pantoprazol in Panrixim is a proton pump inhibitor, which inhibits the last stage of acid formation in the stomach by covalent bonding with the enzyme system (H+, K+)-ATPase at secretory surface of gastric parietal cells.
This mechanism leads to inhibition of both conventional and stimulant gastric acid secretion mechanisms. Binding to the (H+, K+)-ATPase system results in an anti-acid effect lasting more than 24 hours for all doses tested.
Pharmacokinetics:
Peak plasma concentrations of pantoprazole are reached about 2-2.5 hours after absorption into the body. Approximately 98% of pantoprazole will be bound to plasma proteins. Panrixim is extensively metabolised in the liver, mainly via the cytochrome P450 isoenzyme CYP2C19, to desmethylpantoprazol. Small amounts are also metabolised by CYP2D6, CYP3A4, and CYP2C9. The metabolites of Panrixim are eliminated mainly (approximately 80%) in the urine and the remainder is excreted in the bile. The terminal half-life of Panrixim is about 1 hour, longer in patients with hepatic impairment and about 3-6 hours in patients with cirrhosis. Panrixim is indicated for the treatment of:
Gastroesophageal reflux disease (GERD). Gastrointestinal ulcers. Prevention of ulcers caused by non-steroidal anti-inflammatory drugs. Zollinger-Ellison syndrome.
2. Contraindications of Panrixim
Panrixim is contraindicated in the following cases:
Patients with hypersensitivity to Pantoprazol, other benzimidazole derivatives (Lansoprazol, Esomeprazol, Omeprazol and Rabeprazol) or any of the ingredients.
3. Dosage and how to use Panrixim
How to use: Panrixim is used orally. Patients should swallow Panrixim tablets whole. Chewing, breaking, or crushing Panrixim can increase side effects when taken.
Dosage:
Treatment of gastroesophageal reflux syndrome (GERD):
Recommended dose: Take 20-40mg / time / day, for 4 weeks, can last up to 8 weeks. Maintenance dose: 20-40 mg orally per day. In case of relapse: Take 20mg/day. Treatment of peptic ulcers:
Recommended dose: Take 40mg/time/day. Duration of treatment is 2-4 weeks for duodenal ulcer disease and 4-8 weeks for benign gastric ulcer. Prevention of ulcers caused by non-steroidal anti-inflammatory drugs:
Recommended dose: 20mg/day. Treatment of Zollinger - Ellison syndrome:
Initial dose: Take 80mg/day. Patients can take doses up to 240mg/day. If taking more than 80mg/day, it should be divided into 2 times. For patients with liver and kidney failure, it is necessary to consult a doctor for an appropriate dose.
Note: The above dosage of Panrixim is for reference only. The specific dose of Panrixim depends on the condition and the progression of the disease. To get the right dose of Panrixim, patients should consult their doctor or healthcare professional.
4. Panrixim drug interactions
Panrixim has a pH-dependent gastric absorption: Theoretically, the possibility of a pharmacokinetic interaction when pantoprazole is co-administered with drugs with a pH-dependent gastric absorption (eg, ampicillin ester, salts). iron, ketoconazole) will increase or decrease the absorption of Panrixim with increasing gastric pH. Although pantoprazole is extensively metabolized in the liver, primarily by cytochrome P-450 (CYP) isoenzyme 2C19, and to a lesser extent by isoenzymes CYP3A4, CYP2D6 and CYP2C9, clinical trials have shown no clinically significant interactions. There is an important clinical difference between Panrixim and other drugs metabolised by the same isoenzyme. Panrixim has the potential to increase INR and prothrombin time when warfarin is co-administered with proton pump inhibitors, including pantoprazole. Risk of abnormal bleeding and death. Therefore, it is necessary to monitor for an increase in INR when Panrixim is co-administered with Warfarin. In addition, Panrixim may slow the absorption and decrease the bioavailability of proton pump inhibitors (such as lansoprazole and omeprazole). If a combination is required, a proton pump inhibitor should be taken at least 30 minutes before taking Panrixim. To avoid interactions, before being prescribed Panrixim, the patient should inform the doctor about the drugs they are using, including functional foods. The doctor will base on that to prescribe the appropriate Panrixim.
5. Side effects of Panrixim
In general, Panrixim is well tolerated even with short-term and long-term treatment. However, the characteristics of proton pump inhibitors are to reduce gastric acidity and increase the risk of gastrointestinal infections. Therefore, if using Panrixim, patients may also experience some unwanted effects such as:
Common: Fatigue, headache, skin rash, urticaria, muscle pain and joint pain. Uncommon: Asthenia, dizziness, vertigo, pruritus and increased liver enzymes. Rare: Sweating, malaise, peripheral edema, anaphylaxis, maculopapular rash, alopecia, acne, hepatitis, hepatic encephalopathy, jaundice, hypertriglyceridemia, exfoliative dermatitis , hyponatremia, erythema multiforme, angioedema, stomatitis, gastrointestinal disturbances, belching, blurred vision, insomnia, photophobia, somnolence, inhibition, agitation, tinnitus, paralysis positive, confusion, tremor, hematuria, interstitial nephritis, hallucinations, eosinophilia, paresthesia, leukopenia, agranulocytosis, and thrombocytopenia. If you experience these symptoms, the patient should stop using Panrixim and notify the doctor for appropriate treatment.
6. Precautions when using Panrixim
Use of Panrixim in high doses and for a long time (> 1 year), may slightly increase the risk of hip, spine and wrist fractures. This condition mainly occurs in the elderly or in the presence of other risk factors. Panrixim may increase the risk of fracture by 10 to 40%. Patients at risk of osteoporosis should be cared for according to current clinical guidelines and should be adequately supplemented with vitamin D and calcium during treatment with Panrixim. It is advisable to measure magnesium levels before initiating therapy and periodically during treatment in patients who require long-term treatment with Panrixim or who require concomitant administration of Panrixim with Digoxin or other hypomagnesaemic agents. The possibility of a malignant peptic ulcer should be excluded prior to administration of Panrixim because the active ingredient pantoprazole may mask symptoms thereby delaying the diagnosis. Patients may experience mild and transient elevations in serum ALT (SGPT) during treatment with oral panrixim. The safety and effectiveness of Panrixim in children under 18 years of age have not been established. There are no adequate and well-controlled studies of Panrixim in pregnant women. Therefore, women who are pregnant should not take Panrixim. Panrixim is distributed in breast milk. Therefore, it is necessary to discontinue nursing or discontinue Panrixim due to the potential risk to the nursing infant. Panrixim can cause side effects such as dizziness and visual disturbances. If these side effects occur, the patient should not drive or operate machinery. Absolutely do not use when Panrixim has signs of discoloration, mold, watery or expired. Above is all information about Panrixim drug, patients need to carefully read the instructions for use, consult a doctor / pharmacist before using. Absolutely do not arbitrarily buy Panrixim treatment at home because there may be unwanted side effects.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.