This is an automatically translated article.
Ezetimibe + Atorvastatin is indicated for the treatment of hypercholesterolemia and coronary artery disease. On the market today, there is a lot of information about Ezetimibe and Atorvastatin drug products, but it is still incomplete. To learn more about Ezetimibe and atorvastatin, read the article below.1. What is Ezetimibe + Atorvastatin?
Atorvastatin + Ezetimibe is an effective treatment for high blood cholesterol. The product will help reduce low-molecular-weight cholesterol and increase high-molecular-weight cholesterol.1.1. Ingredients of Ezetimibe + atorvastatin
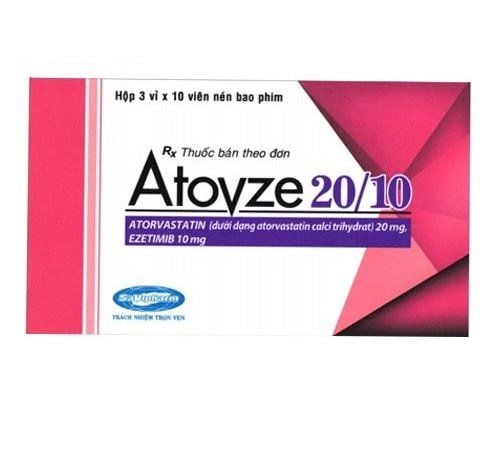
Atorvastatin + Ezetimibe. 1.2. Dosage form and strength Film coated tablets 10mg/10mg: Ezetimibe 10mg and Atorvastatin 10mg. 10mg/20mg film coated tablets: Ezetimibe 10mg and Atorvastatin 20mg. 10mg/40mg film coated tablets: Ezetimibe 10mg and Atorvastatin 40mg. 1.3. Pharmacodynamics of the drug Ezetimibe + Atorvastatin Plasma cholesterol usually has 2 sources: exogenous origin (absorbed from the intestine) and endogenous origin (self synthesis). Ezetimibe and Atorvastatin is a combination drug that reduces plasma cholesterol by both ways of inhibiting absorption and synthesis.
Ezetimibe:
Ezetimibe lowers blood cholesterol by inhibiting cholesterol absorption in the small intestine. Calcium atorvastatin:
Atorvastatin is a synthetic lipid-lowering agent and a 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitor. This enzyme catalyzes the conversion of HMG-CoA to mevalonate and is an early and rate-limiting stage of cholesterol biosynthesis. For patients with homozygous or heterozygous hereditary hypercholesterolaemia, nonhereditary forms of hypercholesterolemia and mixed dyslipidemia, atorvastatin also reduces total cholesterol, lipoprotein cholesterol low molecular weight (LDL-C) and apolipoprotein B (apo B). Atorvastatin will also lower very low molecular weight lipoprotein cholesterol (VLDL-Cholesterol) and triglycerides (TG) and increase high molecular weight lipoprotein cholesterol (HDL-C). 1.4. Pharmacokinetics of Ezetimibe + Atorvastatin Absorption:
Ezetimibe: After oral administration, ezetimibe is also rapidly absorbed and conjugated to form ezetimibe-glucuronide. Maximum plasma concentrations (Cmax) are reached approximately 1-2 hours after oral administration for ezetimibe-glucuronide and about 4-12 hours after oral administration for ezetimibe. Food will have no effect on the bioavailability of ezetimibe. Atorvastatin: Atorvastatin is rapidly absorbed orally and maximum plasma concentrations are reached within 1 - 2 hours. The amount of atorvastatin absorbed and plasma concentrations will increase in proportion to the dose. Atorvastatin tablets are 95-99% bioavailable compared to the solution form. The absolute bioavailability of atorvastatin is about 14% and the inhibitory effect of HMG-CoA reductase is about 30%. The low bioavailability is due to clearance in the gastrointestinal tract prior to entry and by first-pass metabolism in the liver. Distribution:
Ezetimibe: Ezetimibe and ezetimibe-glucuronide will bind to plasma proteins at the rate of 99.7% and 88 ~ 92%. Atorvastatin: The mean volume of distribution of atorvastatin is approximately 381 L. Over 98% of atorvastatin is bound to plasma proteins. The erythrocyte/plasma ratio is about 0.25 indicating little penetration of the drug into erythrocytes. Metabolism:
Ezetimibe: Ezetimibe is metabolised mainly in the small intestine and liver via glucuronide conjugation. Both ezetimibe and ezetimibe-glucuronide are slowly eliminated from plasma by enterohepatic cycling. The half-life of ezetimibe and ezetimibe-glucuronide would be approximately 22 hours. Atorvastatin: Atorvastatin is also extensively metabolised to ortho-, parahydroxy- and multiple oxidation products. In vitro, inhibition of HMG-CoA reductase by ortho- and parahydroxy- metabolites was comparable to that of atorvastatin. Approximately 70% of the inhibitory activity of HMG-CoA reductase in the circulatory system is due to active metabolites. In vitro studies suggest the importance of cytochrome P450 3A4 metabolism of atorvastatin to the liver, due to increased plasma concentrations of atorvastatin in humans following co-administration with erythromycin, an enzyme inhibitor of this enzyme. In vitro studies have also shown that atorvastatin is a weak inhibitor of cytochrome P450 3A4. Concomitant use of atorvastatin did not significantly increase plasma concentrations of terfenadine, a compound that is clearly metabolised by P450 3A4. Therefore, atorvastatin will not significantly alter the pharmacokinetics of other cytochrome P450 3A4 substrates (see Interactions). In animals, the ortho-hydroxy metabolite undergoes glucuronidation. Elimination:
Ezetimibe : Following oral administration of 14C-ezetimibe (20 mg), approximately 93% of ezetimibe is present in plasma. Approximately 78% and 11% were found in feces and urine within 10 days. After 48 hours, the drug was no longer found in the plasma. Atorvastatin: Atorvastatin and its metabolites are also mainly excreted in the bile after hepatic or extrahepatic metabolism. However, the drug does not appear to undergo enterohepatic cycling. The mean plasma half-life of atorvastatin in humans is approximately 14 hours, but the half-life of inhibitory activity for HMG-CoA reductase is 20 to 30 hours due to the contribution of active metabolites. count. Following oral administration, less than 2% of an administered dose of atorvastatin was recovered in the urine.
2. What are the uses of Ezetimibe + Atorvastatin?
Prevention of metabolic cardiovascular diseases:
Atorvastatin + Ezetimibe is indicated to help reduce the risk of cardiovascular events (cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, hospital admissions) due to unstable angina or need for revascularization) in patients with coronary artery disease (CHD) and a history of acute coronary syndrome (ACS) and prior treatment with statins. Primary Hypercholesterolemia: Atorvastatin + Ezetimibe is indicated as adjunct to diet in adult patients with primary hypercholesterolemia (heterozygous familial and non-familial). familial) or mixed hypercholesterolemia, when the use of this combination is appropriate; The patient is also not adequately controlled with statin monotherapy; The patient was being treated with a statin and ezetimibe. Homozygous Familial Hypercholesterolemia (HoFH)
Atorvastatin + Ezetimibe is also indicated as adjunct to diet in patients with homozygous familial hypercholesterolemia (HoFH). Patients may also receive supportive treatments (eg, hemodialysis to remove LDL). 3. Side effects of Atorvastatin+Ezetimibe Gastrointestinal: Diarrhea, constipation, flatulence, abdominal pain and nausea, encountered in about 5% of patients; Central nervous system: Headache (4 - 9%), dizziness (3 - 5%), blurred vision (1 - 2%), insomnia, asthenia; Neuro-muscular and skeletal: Muscle and joint pain; Liver: Liver function test results increased to more than 3 times the upper limit of normal in 2% of patients, but the majority were asymptomatic and resolved when the drug was discontinued. 4. Drug Interactions CYP3A4 Enzyme Inhibitors: Concomitant use with drugs that inhibit the CYP3A4 enzyme may increase plasma concentrations of atorvastatin leading to an increased risk of myopathy and myopathy; Amiodarone: When used with amiodarone, do not exceed 20 mg of atorvastatin/day because of the increased risk of rhabdomyolysis. For patients who must use doses above 20 mg/day to be effective, the doctor may choose another statin drug (such as pravastatin); Coumarin derivatives: Statin drugs will slightly increase the anticoagulant effect of coumarin. For patients receiving coumarin anticoagulants, prothrombin time should be determined before and during atorvastatin therapy.
5. How to use Ezetimibe + Atorvastatin effectively
5.1. How to take Ezetimibe + Atorvastatin?
Patients should follow a low cholesterol diet at the start of treatment and continue to follow this diet for the duration of treatment.
Dosage should be individualized based on plasma lipid levels. Treatment should be initiated with the lowest effective dose of the drug and then, if necessary, adjusted to individual needs and response by increasing the dose at intervals of not less than 4 weeks and should be monitor adverse drug reactions, especially adverse reactions to the muscular system.
5.2. Dosage of Ezetimibe + Atorvastatin Calculated according to Atorvastatin: 10mg, once a day. Permissible dose range: 10-80mg once daily and not related to meals. Maximum: 80mg/day.
The usual dose will be 1 - 4 tablets (Atorvastatin 20mg, Ezetimibe 10mg) / day. Initial use should be at a dose of 1 tablet (Atorvastatin 20mg, Ezetimibe 10mg) / day. After 2 weeks, recheck plasma lipid levels. If necessary, the dose should be adjusted.
Patients with hepatic impairment:
No dosage adjustment is necessary in patients with mild hepatic impairment. Patients with renal impairment:
No dosage adjustment is necessary in patients with mild or moderate renal impairment. However, in patients with severe renal impairment, this drug can only be used if the patient can tolerate atorvastatin at a dose of 5 mg or higher. Caution should be exercised when administering the drug to these patients and the patient should be carefully monitored. Elderly patients:
No dose adjustment is necessary in elderly patients. Patients taking cyclosporin:
For patients taking cyclosporin, this drug can only be used if the patient can tolerate atorvastatin doses of 5 mg or more, but should not take more than 1⁄2 tablets/day. Patients taking Amiodarone or Verapamil:
For patients taking Amiodarone or Verapamil, do not take more than 1 tablet per day. 5.3. Take that dose as soon as you remember it. If it is almost time for your next dose, skip the missed dose and take the next dose only. Do not take a double dose.
5.4. Treatment in case of overdose If an overdose occurs, you need to report it to your doctor immediately, or if you see any unusual symptoms, you need to go to the hospital for timely treatment.
6. Precautions when using Atorvastatin+Ezetimibe Elderly (over 70 years old); CKD; Uncontrolled hypothyroidism; You or your family also have a history of myopathy; There is a history of muscle toxicity with the use of Statins or Fibrates; Alcoholism. 6.1. Use for pregnant or lactating women Consult a doctor immediately before use in pregnant or lactating women.
6.2. Use for Drivers and Machine Operators Consult a physician immediately before driving or operating machinery.
7. How should you store Ezetimibe + Atorvastatin? You should also store it at room temperature, away from moisture and light. Do not store in the bathroom or in the freezer. You should keep in mind that each medicine may have different storage methods. Therefore, you should carefully read the storage instructions on the packaging or ask your pharmacist. Keep the medicine out of the reach of children and pets.
You should also not throw medicine down the toilet or plumbing unless you tell it to. Instead, dispose of your medicine properly when it is past its expiration date or cannot be used. You may need to consult your pharmacist or local waste disposal company about how to safely dispose of your medication.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.