This is an automatically translated article.
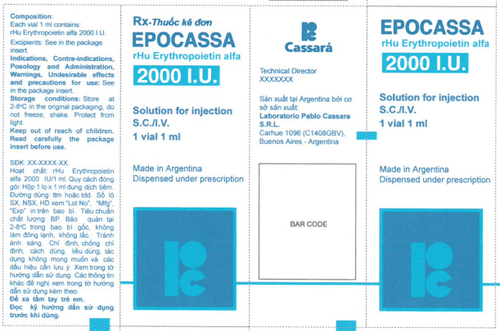
Epoetin beta is indicated for the treatment of anemia due to symptomatic chronic renal failure in patients on dialysis and renal replacement. There is a lot of information on the Epoetin beta drug product on the market today, but it is still incomplete. To better understand Epoetin beta drug, let's learn more in the article below.1. What is Epoetin beta drug?
Epoetin beta is used to treat patients with symptomatic anemia associated with chronic kidney disease and to treat chemotherapy-related anemia in cancer patients.Epoetin beta injection is very similar to Epoetin alfa and works the same way as injecting Epoetin alfa into the body.
These drugs work by signaling the bone marrow to make more red blood cells. This medicine is very similar to a natural substance in your body called Erythropoietin, which prevents anemia.
The drug is formulated for a variety of concentrations from 500 to 50,000 international units (IU), as a solution for injection such as:
Powder form in multi-dose vials and solvent for injection. Premixed single dose syringe. The biological effects of Epoetin beta have also been demonstrated following intravenous and subcutaneous administration in various animal models in vivo (normal and uremic rats, polycythemia vera and dogs). After administration of Epoetin beta drug, the number of red blood cells, hemoglobin and reticulocytes as well as the 59Fe binding rate all increased.
An increase in 3H-thymidine binding was found in vitro to splenic nucleated red blood cells (cultured mouse spleen cells) after incubation with Epoetin beta.
Studies in human bone marrow cell cultures also show that Epoetin beta specifically stimulates erythropoiesis and does not affect leukocyte formation. No cytotoxic effects of Epoetin beta were found on human bone marrow or skin cells.
Pharmacokinetic studies in healthy volunteers and uremic patients have shown that the half-life of Epoetin beta after intravenous administration is 4 to 12 hours and the volume of distribution is 1 to twice the plasma volume. Similar results have also been observed in laboratory animals in normal and hyperuricemic rats.
Following subcutaneous administration of Epoetin beta to patients with uremia, prolonged absorption leads to stable serum concentrations, with maximum concentrations being reached after approximately 12-28 hours.
The bioavailability of Epoetin beta after subcutaneous administration will be about 23 to 42% compared to intravenous administration.
Distribution: Pharmacokinetic studies in healthy volunteers and uremia patients have shown that the volume of distribution corresponds to one to two times the plasma volume.
Elimination:
Pharmacokinetic studies in healthy volunteers and uremic patients have shown that the elimination half-life of intravenous Epoetin beta ranges from 4 to 12 hours. Following subcutaneous administration of Epoetin beta to uremia patients, the half-life was longer than after intravenous administration and averaged 13 to 28 hours. Pharmacokinetics in Special Patient Populations: No formal studies on the effects of hepatic impairment on the pharmacokinetics of Epoetin beta have been performed.
2. What are the uses of Epoetin beta?
The drug is indicated in the following cases:
Treatment of anemia (to raise or maintain red blood cell levels and reduce the need for blood transfusions) caused by chronic renal failure (whether or not in patients requiring dialysis). hemodialysis), for patients on peritoneal dialysis (to reduce or eliminate the need for blood transfusion). Prevention of anemia in premature infants with birth weight between 750 and 1500g and gestational age less than 34 weeks. Treatment of anemia by chemotherapy in patients with non-bone marrow malignancies and zidovudine-related anemia in HIV-positive patients. Treatment of moderate anemia (but not iron deficiency) in elective preoperative (non-cardiac or vascular) patients to increase blood output for autologous transfusion and reduce transfusion requirements fellow. Treat patients with moderate anemia (Hb 10 – 13 g/dl [6.21 – 8.07 mmol/l], no iron deficiency) (4 or more blood units for women or 5 or more units for men). 3. Epoetin beta side effects Common side effects include:
Headache; Convulsions ; Hypertension ; Thrombosis in blood vessels; Coagulation; Temporary increase in platelet count; flu symptoms, such as chills, muscle aches, hyperkalemia, skin rash; Hypertensive crisis for symptoms such as, headache and confusion, convulsions (patients with normal or low blood pressure); Anaphylactic shock is rare. Not everyone experiences these side effects. There may be some side effects not listed above. If you are concerned about certain side effects consult your doctor or pharmacist.
4. Epoetin Beta drug interactions
4.1. What drugs may interact with Epoetin beta?
Although there are some medicines that should not be used with this medicine, in other cases two different medicines can still be used together even if there is still the possibility of an interaction. In this case, your doctor may want to change the dosage or take other precautions if it may be necessary.
Use of this medicine for some of the medicines below is generally not recommended, but in some cases it may be necessary. If these two drugs are prescribed to you, your doctor will usually also change the dosage or determine how often you should take them. This drug helps to counteract the hypotensive effects of ACE inhibitors and angiotensin-II receptor antagonists and increases the risk of hyperkalemia.
4.2. Can food or alcohol interact with Epoetin beta? Some medications should not be taken with meals or when eating certain foods because of possible drug interactions. Drinking alcohol or tobacco along with certain medications can also cause interactions. Discuss your drug use with food, alcohol, or tobacco with your healthcare provider.
4.3. What health conditions may interact with Epoetin beta?
Any of your other medical conditions may affect the use of this medicine. Always tell your doctor if you have other health problems, especially:
High blood pressure; History of seizures; Increased platelets; Chronic liver disorders; Ischemic disease ; Melanoma ; Epileptic; Latest MI or CVA; Fe deficiency; The infection; Inflammatory disorders; Hemolysis and aluminum toxicity may reduce the response to Epoetin beta; Regularly monitor platelet counts and serum potassium levels; Control the hematocrit level; Uncontrolled hypertension: Monitor BP, Hb and electrolytes; Anemia (eg, megaloblastic or folic acid): Iron supplements as needed. Thrombocytosis: monitor the platelet count within weeks 1 and 8. 5. How to use and dose Epoetin beta is effective 5.1. Instructions for using Epoetin beta medicine Wash your hands first!
Step 1: Remove the syringe from the case and check that the solution is clear, colorless and especially free of residue. Remove the cap from the syringe.
Step 2: Take the needle out of the case, insert it into the syringe and remove the cap of the needle.
Step 3: Remove air from the syringe and needle by holding the syringe upright and gently pushing the plunger upwards. Push the plunger until the prescribed dose is reached in the syringe.
Step 4: Wipe the skin at the injection site with alcohol-soaked cotton. Skin folds should be created by pinching the skin between the thumb and index finger. Hold the syringe close to the needle, and quickly insert the needle into the skin fold firmly. Inject the drug solution. Remove the needle quickly and apply pressure to the injection site with a dry, sterile gauze pad.
5.2. Dosage of Epoetin beta Drug Treatment of patients with anemia due to chronic renal failure
The solution can be injected subcutaneously or intravenously. In the case of intravenous injection, you need to inject the solution within 2 minutes, for example in dialysis patients, it should be administered via an arteriovenous bridge when dialysis is complete.
For non-dialysis patients, the subcutaneous route should always be preferred to avoid rupture of peripheral veins.
The aim of treatment is to increase hematocrit up to 30-35% with a weekly increase of at least 0.5%. The value of 35% should not be exceeded.
In the case of hypertension or pre-existing cardiovascular disease, the cerebral or peripheral pulse, the weekly increase in hematocrit and the target hematocrit should be determined individually for each patient according to the clinical picture. For some patients the optimal hematocrit may be less than 30%.
Treatment with the drug will be divided into 2 phases as follows:
* Treatment phase
Subcutaneous injection: The starting dose is 3 x 20 IU/kg body weight per week. The dose may be increased every 4 weeks by 3 x 20 IU/kg for one week if the hematocrit is not increased sufficiently (< 0.5% per week). The weekly dose may be divided into daily doses. Intravenous: The starting dose is 3 x 40 IU/kg body weight per week. After 4 weeks the dose can be increased to 80 IU/kg - 3 times a week - and if necessary continue to increase by 20 IU/kg three times a week every month. For both routes of administration, the maximum dose should not exceed 720 IU/kg per week.
* Maintenance phase
To keep the hematocrit between 30-35%, first reduce the dose to half of the current dose. After that, the dose will be adjusted every week or two according to the individual patient (maintenance dose). The treatment with conventional oral will be prolonged. However, if necessary, it can be stopped suddenly at any time. Once-weekly dosing data have also been established based on clinical studies with a treatment duration of 24 weeks. Prevention of anemia in premature infants
The drug is used by subcutaneous injection at a dose of 3 x 250 IU/kg body weight per week.
Treatment with the drug should begin as soon as possible and preferably on the third day after delivery. Premature infants who received a blood transfusion at the start of drug therapy may not be as effective as those who did not receive a blood transfusion.
The treatment should last about 6 weeks.
Treatment of symptomatic anemia in patients with cancer
Solution used for subcutaneous injection; The weekly dose can be given as a single injection or divided into 3 to 7 single doses.
The recommended starting dose is 30,000 IU/week (equivalent to approximately 450 IU/kg body weight per week and based on an average weight patient).
The drug is also indicated if the hemoglobin value is ≤ 11g/dl (6.83 mmol/l). The hemoglobin level should not exceed 13g/dl (8.07 mmol/l) (See Pharmacodynamics).
If, after 4 weeks of treatment, the hemoglobin value increases by at least 1g/dl (0.62 mmol/l), the patient's current dose should be continued. If the hemoglobin value does not increase by at least 1 g/dl (0.62 mmol/l), a doubling of the weekly dose should be considered. If, after 8 weeks of treatment, the hemoglobin value does not increase to at least 1g/dl (0.62 mmol/l), response is unlikely and treatment should be discontinued.
Treatment should be continued until 4 weeks after the end of chemotherapy.
The maximum dose should not exceed 60,000IU per week.
Once the patient's therapeutic goal has been achieved, the dose should be reduced by 25% to 50% to maintain the hemoglobin at the level achieved. If necessary, further dose reduction is required to ensure that the hemoglobin value does not exceed 13 g/dl.
If hemoglobin increases above 2g/dl (91.3 mmol/l) in 4 weeks, the dose should be reduced by 25% to 50%.
5.3. What should you do in case of an emergency or overdose? In the event of an emergency or overdose, call 911 immediately or go to the nearest local health station.
5.4. What should you do if you miss a dose? If you forget to take a dose, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and take your next dose at the scheduled time. Do not use double the prescribed dose.
6. Caution/Warning when taking Epoetin beta 6.1. Before taking Epoetin beta Tell your doctor if you are allergic to Epoetin beta or any other medications. Tell your doctor if you are pregnant and plan to become pregnant or are breast-feeding. Tell your doctor about all medications you are taking, including herbs and supplements. Tell your doctor if you have uncontrolled high blood pressure. 6.2. Things to keep in mind if you are pregnant or breast-feeding There are not enough studies to determine the risks of using this medicine during pregnancy or breast-feeding. Always consult your doctor before taking any medication to weigh the benefits and risks.
7. Preservation of Epoetin beta medicine Store the medicine at a temperature between 2 and 8oC in the refrigerator. Keep the prefilled vial or syringe in the paper box to protect it from light.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.