This is an automatically translated article.
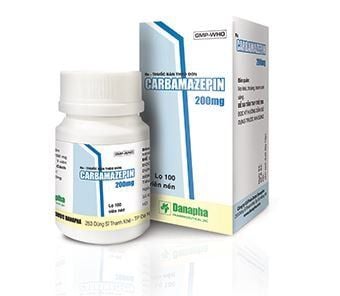
Carbadac is made in the form of tablets, the main ingredient is Carbamazepine. The drug is used in the treatment of epilepsy, manic episodes, alcohol withdrawal syndrome, ...
1. What are the uses of Carbadac?
1 Carbadac tablet contains Carbamazepine 200mg as the main ingredient. Carbamazepine is an antiepileptic drug, related to tricyclic antidepressants. Carbamazepine has anticonvulsant effects associated with decreased neuronal excitability and synaptic blockade. In addition, Carbamazepine is also effective against paroxysmal pain in patients with trigeminal neuralgia, epilepsy, and alcohol withdrawal. At the same time, Carbamazepine increases the seizure threshold, reduces the risk of spasticity, reduces alcohol withdrawal symptoms.
Indications for the use of Carbadac:
Treatment of partial seizures with complex symptoms (psychomotor epilepsy, temporal lobe epilepsy); Treatment of acute manic episodes, maintenance treatment of bipolar affective disorders to prevent or reduce relapses; Treatment of alcohol withdrawal syndrome; Treatment of idiopathic trigeminal neuralgia, trigeminal neuralgia due to multiple sclerosis; Treatment of diabetic neuropathy that causes pain; Treatment of central diabetes insipidus, polyuria and polydipsia of neurohormonal origin. Contraindications to the use of Carbadac:
Patients with hypersensitivity to Carbamazepine, tricyclic antidepressants; Patients with bone marrow failure; Concomitant use with MAOIs (should stop taking MAO drugs at least 14 days before).
2. How to take and dose of Carbadac
Usage: Orally.
Dosage: Treatment should be started with the lowest dose, then gradually increased until maximum effect is achieved. Once seizures are well controlled, the dose can be gradually reduced to the lowest effective dose. It may be useful to determine blood levels of the drug while maintaining optimal dosing levels. Where Carbadac is added to another antiepileptic drug, the drug should be introduced gradually during maintenance therapy or if the dose of the other drug needs to be adjusted.
Specific dosage for each disease group and patient population is as follows:
Treatment of epilepsy:
Adults: Start treatment with a dose of 100-200mg/time x 1-2 times/day, the dose should be increased. gradually until the maximum dose is reached (400mg/time x 2-3 times/day). Up to 1600mg/day or even 2000mg/day may be used in some patients; Children: Use dose 10-20mg/kg body weight daily. Specifically: Children ≤ 1 year old: Use a dose of 100-200mg/day; Children 1 - 5 years old: Use a dose of 200 - 400mg/day; Children 6 - 10 years old: Use a dose of 400 - 600mg/day; Children 11 - 15 years old: Use 1000mg/day; In children under 4 years of age, treatment should be initiated at a dose of 20-60mg/day, increasing the dose from 20-60mg/day. For children over 4 years of age, treatment should be started at 100 mg/day, increasing to 100 mg/week. If alternative treatment is with rectal suppositories, the dose should be increased by 25% to the level mentioned above, the maximum dose should not exceed 1000mg. Treatment of neuralgia V:
Initial dose: 200-400mg/day. The dose should be increased slowly until the pain is gone (usually at a dose of 200mg/time x 3-4 times/day). Thereafter, the dose of Carbadac should be gradually reduced to the lowest possible maintenance dose; The starting dose of 100mg/time x 2 times/day can be applied to the elderly. Treatment of alcohol withdrawal syndrome:
Average dose: 200mg/time x 3-4 times/day. In severe cases, the dose should be increased in the first days (up to 400mg/time x 3 times/day); Initiating treatment in severe cases should be combined with carbamazepine with sedative/hypnotic drugs (eg, clomethiazol, chlordiazepoxide). Once the acute phase is over, Carbamazepine is continued as monotherapy. Treatment of manic episodes and prevention of manic - depressive states (bipolar disorder):
Use a dose of about 400 - 1600mg/day. Dosage should be 400 - 600mg/day, divided into 2 - 3 times; The dose should be increased rapidly during acute manic episodes, increasing the dose slightly if bipolar disorder is prevented for best tolerability. Missed dose: If you forget to take a dose of Carbadac, you should take it as soon as you remember. If the interval between the next dose is too short, the patient can skip the missed dose and continue as scheduled, without the need to take a double dose to make up for the missed dose.
Overdose: When using Carbadac drug overdose, patients may experience symptoms of the central nervous system, respiratory tract and cardiovascular system. Specifically:
Central nervous system: Disorientation, somnolence, nervous depression, agitation, color blindness, hallucinations, coma, slurred speech, nystagmus, dysarthria, anterior hyperreflexia - after hyporeflexia, myoclonus, convulsions, psychomotor disturbances, hypothermia; Respiratory tract: Pulmonary edema, respiratory failure; Circulatory system: Hypotension, sometimes hypertension, tachycardia, syncope with cardiac arrest, QRS complex disturbances; Digestive system: Decreased intestinal motility, vomiting, slow gastric secretion; Urology - genitourinary: Oliguria, urinary retention, water retention, water intoxication (similar to the effect of ADH); Laboratory tests: Metabolic acidosis, hyponatremia, possible hyperglycemia, increased muscle creatinine phosphokinase. There is currently no specific antidote for carbamazepine overdose. Initial management depends on the individual patient's condition: Transfer to hospital -> determine blood drug levels to verify Carbamazepine toxicity and extent of overdose -> Aspiration, gastric lavage, charcoal administration active. Patients need special health care, close monitoring of cardiovascular and electrolyte balance. Some specific guidelines include:
Lowering blood pressure: Administer intravenous dopamine or dobutamine; Arrhythmia : Treatment depends on each specific case; Seizures: Use a benzodiazepine (such as diazepam) or another antiepileptic drug such as phenobarbital (with caution because it may increase respiratory depression) or use paraldehyde; Hyponatremia (water intoxication): Should limit the introduction of water into the body and slow infusion, with caution when using 0.9% NaCl solution intravenously. These measures can be helpful in preventing brain damage. Coal column transfusion, increased diuresis, hemodialysis and peritoneal dialysis are also effective; It should be noted that recurrent or worsening symptoms may appear on the 2nd and 3rd day after overdose due to slow absorption.
3. Carbadac side effects
When using Carbadac, patients may experience some side effects as follows:
Central and peripheral nervous system: Common: Dizziness, fatigue, somnolence, ataxia, headache, visual disturbances (color blindness), double vision; Rare: Involuntary movements (posturethrosis, tremor, chorea, oral-facial dyskinesia, myoclonus, dystonia), nystagmus; Very rare: Ocular disorders, peripheral neuritis, speech disorders (dysphagia, slurred speech), paresthesias; Psychiatric: Hallucinations (visual, auditory), loss of appetite, depression, restlessness, agitation, agitated behavior, confusion, activation of mental disorders; Skin: Common: Allergic skin reactions, urticaria (may be more severe); Rare: Systemic lupus erythematosus, Stevens-Johnson syndrome, exfoliative dermatitis and erythema; Very rare: Photosensitive reactions, purpura, toxic epidermal necrolysis, erythema multiforme and maculopapular rash, acne, skin pruritus, skin pigmentation changes, alopecia, profuse sweating foul, hirsutism (female); Blood: Common: Leukopenia, thrombocytopenia, eosinophilia; Rare: Lymphadenopathy, leukocytosis; Very rare: Aplastic anemia, megaloblastic anemia, agranulocytosis, aplastic anemia, erythrocytosis, acute porphyria, hemolytic anemia, anemia folic acid deficiency; Liver: Common: Increased GGT (due to decreased liver enzymes), increased alkaline phosphatase; Rare: Increased transaminases, cholestasis, jaundice, hepatocellular parenchymal inflammation, mixed hepatitis; Very rare: Granulomatous hepatitis; Gastrointestinal: Common: Nausea, vomiting, dry mouth; Rare: Diarrhea, constipation; Very rare: Abdominal pain, stomatitis, glossitis, colon irritation, hypersensitivity reactions; Hypersensitivity: Rare: Late organ hypersensitivity presenting with fever, vasculitis, rash, lymphadenopathy, arthralgia, lymphoma-like disorder, leukopenia, eosinophilia, laboratory tests abnormal rash, hepatosplenomegaly,...; Very rare: Anaphylaxis, aseptic meningitis, myoclonus and peripheral eosinophilia. The drug should be discontinued if these symptoms of hypersensitivity appear; Cardiovascular: Rare: Cardiac conduction disturbances; Very rare: Bradycardia, arrhythmia, pulse collapse, atrioventricular block with syncope, hypotension or hypertension, congestive heart failure, coronary insufficiency, thromboembolic disease, thrombophlebitis circuit; Endocrine and Metabolic: Common: Edema, weight gain, fluid retention, hyponatremia and decreased fluid concentration due to ADH-like effects, water intoxication, vomiting, headache, lethargy, confusion, psychiatric disorders terrible; Rare: gynecomastia or lactation in men, abnormal thyroid function tests (lower L-thyroxine (FT4, T4, T3) and increased TSH), bone metabolism disorders, hypercholesterolemic osteomalacia; Urogenital - genitourinary: Interstitial nephritis, renal failure, signs of renal dysfunction (hematuria, oliguria, albuminuria, BUN elevation), urinary frequency, urinary retention, sexual dysfunction/impotence ; Senses: Taste disturbance, tinnitus, conjunctivitis, cataracts, lowered hearing threshold; Musculoskeletal: Cramps, myalgia, arthralgia; Respiratory: Pulmonary hypersensitivity with dyspnea, fever, focal pneumonia/pneumonia. When experiencing any side effects of Carbadac, the patient should immediately notify the doctor to receive advice on how to handle and respond appropriately.
4. Be careful when using Carbadac
Some notes for patients to remember before and while taking Carbadac:
Caution when using Carbadac in patients with glaucoma, heart failure, liver failure and kidney failure; Use caution when using Carbadac in children under 6 years of age; Carbadac should be used with caution in pregnant and lactating women, when driving a vehicle or operating machinery; Avoid concomitant use of Carbadac with MAO inhibitors. At least 14 days after discontinuation of MAOIs, the patient can start using Carbamazepine; Caution should be exercised when discontinuing carbamazepine therapy in epileptic patients; You should not eat grapefruit or drink grapefruit juice while taking Carbadac.
5. Carbadac drug interactions
Carbadac drug may interact with other drugs, leading to affecting the effectiveness of the drug or increasing side effects,... Some of Carbadac's drug interactions include:
Due to the effect on The liver enzyme mono-oxygenase system, so Carbamazepine can lower the concentration or make the effect of some drugs metabolised through this system. Therefore, it may be necessary to change the dosage of the following drugs to meet clinical requirements: Clobazam, clonazepam, ethosuximide, valproic acid, primidone, alprazolam; corticosteroids (such as prednisolone, dexamethasone); oral contraceptives (need selection of appropriate methods of contraception); cyclosporin, doxycycline, felodipine, digoxin, haloperidol, imipramine, methadone; theophylline; oral anticoagulants (phenprocoumon, warfarin, dicoumarol); Carbamazepine may increase and decrease the concentration of mephenytoin; Drugs that may increase carbamazepine levels include: Erythromycin, troleandomycin, josamycin, isoniazid, fluoxetine, verapamil, diltiazem, dextropropoxyphene, viloxazine, danazol, cimetidine, acetazolamide, desipramine and nicotinamide (in adults), and only in high doses . The increased concentration of Carbamazepine in the blood can lead to side effects such as ataxia, dizziness, somnolence, double vision, ... so it is necessary to adjust the dose of Carbadac drug accordingly or monitor the concentration. drugs in the blood; Increased possibility of isoniazid hepatotoxicity if carbamazepine is used in combination with isoniazid; Co-administration of Carbamazepine with lithium, metoclopramide or with neuroleptics (eg, haloperidol, thioridazine) may increase neurological reactions; Carbamazepine concentrations may be decreased by phenytoin, primidone, phenobarbital, progabide, theophylline and possibly by clonazepam, valproic acid, valpromide. Carbamazepine dosage can be adjusted if necessary; Concomitant use of carbamazepine with diuretics such as hydrochlorothiazide, furosemide may lead to hyponatremia; Carbamazepine may have an antagonistic effect on non-depolarizing muscle relaxants such as pancuronium. Therefore, higher doses of these drugs may be required, in conjunction with close monitoring of the patient's health; Isotretinoin may alter the bioavailability and clearance of carbamazepine. Carbamazepine levels should be monitored when co-administered with isotretinoin; Carbamazepine can reduce alcohol tolerance, so patients should not drink alcohol while taking it. When prescribed Carbadac, the patient should take the drug exactly as directed by the doctor. Patients must not arbitrarily change the dose, time of use, method of taking drugs, ... without the permission of the doctor to avoid dangerous adverse reactions.
Follow Vinmec International General Hospital website to get more health, nutrition and beauty information to protect the health of yourself and your loved ones in your family.