This is an automatically translated article.
Busmocalm, on the World Health Organization's list of essential medicines, is an anticholinergic drug used to treat abdominal cramps, esophageal spasms, renal colic and bladder spasms, etc..
1. What is the effect of Busmocalm?
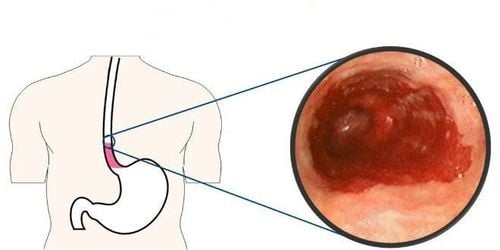
Busmocalm - 10mg has the main ingredient is Hyoscine butylbromide with a concentration of 10mg. Busmocalm is used in the treatment of diseases such as:The drug is indicated to relieve spasms of smooth muscle of the urogenital or gastrointestinal tract. The ingredient Hyoscine Butylbromide is also used in combination with other medications to treat symptoms such as abdominal pain, bloating, indigestion, cramping, diarrhea associated with irritable bowel syndrome (a disorder that affects affects the large intestine) and peptic ulcers (open sores that occur on the inner lining of the stomach and the upper part of the small intestine). Used in the prevention and treatment of dysmenorrhea. It is also used to improve respiratory secretions. Mechanism of action:
Main ingredient Hyoscine butylbromide is an anticholinergic agent, belonging to the group of muscarinic antagonists that works to block smooth muscle contractions stimulated by acetylcholine in the gastrointestinal tract, antispasmodic smooth muscle in the gastrointestinal tract. digestive tract, biliary tract and genitourinary tract.
2. Dosage and usage
How to use: Busmocalm is prepared in the form of sugar coated tablets and used orally, note that when patients take the drug, they should take the whole pill and drink it with plenty of water for the drug to be effective.
Dosage:
Recommended dose for adults and children over 12 years old use 2 tablets, 4 times a day.
In the treatment of symptoms of irritable bowel syndrome, the dose applied in the first time is 1 tablet 3 times a day. After that, the dose can be increased to 2 tablets, 4 times a day as needed. For children from 6 to under 12 years old use 1 tablet 3 times / day. For elderly patients, the usual dose of the drug can be applied because current clinical trials show that patients over 65 years of age using the drug have not recorded any typical side effects, so it may not be necessary to change the dose. change dose. Note: Do not use the drug for children under 6 years old.
Overdose and treatment
Overdose: Common manifestations of drug overdose include urinary retention, dry mouth, skin redness, heart rhythm disturbances, inhibition of intestinal motility and visual disturbances. Treatment: Usually the doctor will prescribe treatment according to the symptoms. Specifically: For severe poisoning, the patient will be prescribed gastric lavage with activated charcoal, for patients with glaucoma symptoms, Pilocarpine will be used for topical treatment. In case of respiratory paralysis, the patient will be intubated and given artificial respiration, when experiencing symptoms of urinary retention, a urinary catheter will be inserted.
3. Contraindications
Do not use the drug in patients who are allergic to the ingredient Hyoscine butylbromide or to any of the ingredients in Busmocalm. Do not use in patients with severe myasthenia gravis. Contraindicated to use the drug in patients with ulcerative colitis. Patients with glaucoma or mechanical intestinal obstruction. The patient has functional bowel paralysis. The patient has a pathological tachyarrhythmia problem. Patients with obstructive prostate enlargement or achalasia.
4. Side effects
Common side effects include:
Skin reactions with itching and hives, causing hives. Effects on the cardiovascular system with the most common symptom being tachycardia. Effects on the digestive system are manifested as dry mouth. The drug causes drowsiness, vision changes, glaucoma trigger, and severe allergies. Rare reactions such as urinary retention. Rare photo reactions such as anaphylaxis, anaphylaxis, rash, erythema, dyspnea. How to handle unwanted side effects: When experiencing serious side effects, the patient should stop taking the drug and use other more suitable treatment methods.
5. Caution
Caution should be exercised when using the drug in patients with a predisposition to drugs containing methyl hydroxybenzoate and propyl hydroxybenzoate preparations, because in this case there is a high risk of unwanted side effects. Use with caution in patients with rare hereditary problems of galactose and fructose intolerance, Lapp lactase deficiency, sucrase - isomaltase or glucose - galactose malabsorption. The drug should be used with caution in patients with undiagnosed and untreated narrow-angle glaucoma, so the patient should consult an ophthalmologist. If there are symptoms such as eye redness accompanied by a decrease in eye vision after using Busmocalm. The drug should be used with caution in patients at risk of bowel or urethral obstruction due to the risk of complications from anticholinergics. Use with caution in patients with fever because the drug can reduce the ability to sweat. The drug should be used with caution in patients with thyrotoxicosis, heart failure, cardiac surgery, and cardiac surgery because the drug may aggravate tachycardia. During the use of the drug, if the patient experiences problems such as unexplained abdominal pain accompanied by symptoms such as fever, nausea, vomiting or changes in bowel movements, when the patient presses on the abdomen, pain, low blood pressure, fainting or blood in the stool, you need to consult a doctor immediately to take measures. For pregnant women: Currently, animal studies show that the drug has no direct or indirect effects on fetal development. However, these data are incomplete and limited. Therefore, pregnant women should not use the drug or consult a doctor before using it. For women who are breast-feeding: It has not been confirmed whether the components of the drug can be excreted in breast milk, so to avoid affecting the development of the child, the mother should not use the drug during breastfeeding. suck. Effects of the drug on the ability to drive and use machines: Because the drug causes visual disturbances, caution should be exercised when used with people performing dangerous jobs and requiring high concentration. .
6. Drug interactions
Before taking Busmocalm, patients should inform their doctor about the drugs they are using or have used recently to avoid causing drug interactions between Busmocalm and other drugs, affecting the effective use. medication or cause unwanted side effects. Hyoscine butylbromide may potentiate the anticholinergic effects of tricyclic and tricyclic antidepressants, antihistamines, quinidine, cimetidine, antipsychotics such as butyrophenones, phenothiazines and other anticholinergics. Concomitant use with dopamine antagonists such as metoclopramide may affect the effect of both drugs on the gastrointestinal tract. Concomitant use with beta sympathomimetic drugs can cause side effects such as arrhythmia. Concomitant use with antacids or antidiarrheal drugs may reduce the absorption of anticholinergic drugs to the point of ineffective treatment. If it is necessary to use it, it should be at least 1 hour apart from the time of taking these two drugs. CNS depressant) of Butylscopolamine Acetazolamide : Acetazolamide may increase the CNS depressant (CNS depressant) activities of Butylscopolamine Acetophenazine: Acetophenazine may increase the activity of Butylscopolamine causing central nervous system depression (CNS depressant) Aclidinium : The risk or severity of adverse events may be increased when Butylscopolamine Adenosine: The risk or severity of Tachycardia may be increased when Adenosine is combined with Butylscopolamine. Alloin: The therapeutic efficacy of Aloin may be reduced when used in combination with Butylscopolamine Ambenonium: The therapeutic effect of Butylscopolamine may be reduced when used in combination with Ambenonium Bendroflumethiazide: Bendroflumethiazide serum concentrations may be increased increased when it is combined with Butylscopolamine Baclofen : Baclofen may increase the activity of Butylscopolamine causing central nervous system depressant (CNS depressant) Reference source: en.wikipedia.org; go.drugbank.com.