This is an automatically translated article.
Brulamycin is an aminoglycoside antibiotic derived from Streptomyces tenebarius and is used to treat bacterial infections, especially Gram-negative infections.1. What effect does Brulamycin have?
What does Brulamycin do? Brulamycin has the main ingredient Tobramycin, which is on the World Health Organization's list of essential drugs, belonging to the group of drugs used to treat eyes and ears, nose and throat. Doctors usually prescribe Brulamycin in the following cases:
Treatment of inflammatory eye conditions that have responded to steroids and when there is a superficial bacterial infection of the eye or there is a risk of eye infection. The drug is indicated for use in the treatment of urinary tract infections, infections of the circulatory system and blood, infections of bones, skin and soft tissues, infections of the central nervous system, infections of the lower respiratory tract. caused by susceptible bacteria. Brulamycin is used effectively in the treatment of eye infections such as keratitis, eyelid inflammation, conjunctivitis, trachoma, stye .. Mechanism of action: Tobramycin is an antibiotic drug. The 4,6-deoxystreptamine (DOS) ring contains an aminoglycoside that is active against Gram-negative bacteria and a variety of Gram-positive bacteria. The drug inhibits protein synthesis in susceptible bacteria by irreversibly binding to the 30s ribosomal subunit, preventing the growth and spread of pathogenic bacteria.
2. Dosage and way of taking Brulamycin
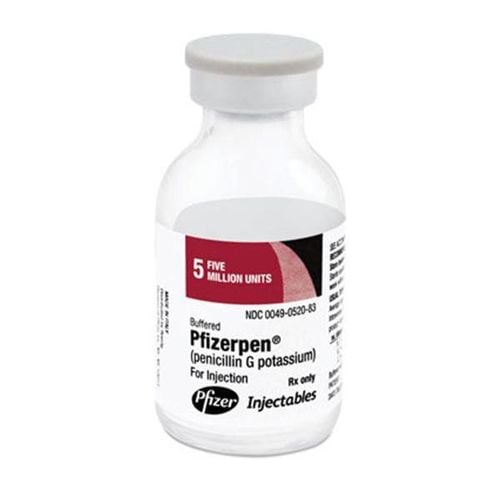
Usage: The drug is prepared in the form of eye drops, injection form.
Dosage: Depending on the progression of the patient's medical condition, the doctor may prescribe different doses of drugs.
For eye drops
In the treatment of mild and moderate infections use 1 to 2 drops a day 3 to 4 times In the treatment of severe infections use 1 to 2 drops every hour times until the disease gets better, then gradually reduce the number of times of taking the drug. Note: Do not share the vial with more than one person to avoid the risk of cross-contamination and do not use the medicine more than 15 days after the first opening.
For injectable or infusion drops
For intramuscular (IM) use
In adults with normal renal function the recommended dose is 1 mg/kg every 8 hours. Duration of treatment is 7 to 10 days for patients with severe infections, the dose can be increased to 5 mg. However, as soon as the symptoms of the disease improve, the patient should reduce the dose of the drug to 3 mg as soon as possible. For children 3 to 5 mg/kg/day, every 8 to 12 hours For infants weighing 1.5 to 2.5 kg, 2 mg/kg every 12 hours . Use in intravenous infusion (IV)
Patients only use the intravenous line when it is not possible to use the intramuscular route, the drug concentration when mixed does not exceed 1mg/ml (0.1%), Time of infusion 1 to 2 hours for patients with renal impairment, the dose should be adjusted according to the level of creatinine clearance.
Contraindications:
Do not use brulamycin in patients who are allergic to Tobramycin or to any of its ingredients. Do not use the drug in patients with a history of severe myasthenia gravis.
3. Overdose and treatment of Brulamycin
Manifestations of overdose : When using an overdose, patients are at risk of serious side effects such as kidney or hearing toxicity, neuromuscular blockade affecting respiratory ability, causing drowsiness. , dizziness , irregular breathing , lips, fingernails, skin with signs of pale blue.
Treatment: Using supportive measures and symptomatic treatment such as hemodialysis can help remove excess drug toxins from the body.
4. Side effects when using Brulamycin
In patients with normal renal function when not exceeding the recommended dose and duration of treatment, the incidence of adverse reactions is very low. For the elderly and patients with kidney failure, when using an overdose of the drug and the duration of treatment, the risk of side effects will increase. Common side effects include dizziness, hearing loss, and nystagmus. Some other side effects such as thrombocytopenia, fever, urticaria, vomiting, nausea, anemia, agranulocytosis, unconsciousness, loss of orientation and pain at the injection site . Other less common side effects include nephrotoxicity, neuromuscular toxicity, and hypersensitivity reactions More serious abnormalities that may occur with tobramycin include: Increased serum transaminases (SGOT-SGPT) and lactic dehydrogenase, decreased serum calcium, magnesium, sodium and potassium, leukopenia, leukocytosis, and eosinophilia.
5. Be careful when using Brulamycin
Caution should be exercised when using Brulamycin in the following cases:
Because the drug is excreted in the urine, it should be used with caution in patients with impaired renal function. In the process of using the drug, it is necessary to monitor the patient carefully, because the drug affects kidney function, nervous system and affects hearing. To avoid cross-infection, the drug should not be used by more than one person. After opening the cap of the vial, the maximum use time is 15 days, after 15 days, the patient should not continue to use the drug. It should only be used for infants in case of a life-threatening emergency, in addition, the drug should not be used for children without a doctor's prescription. Avoid concomitant use with other neurotoxic or nephrotoxic drugs such as aminoglycosides (amikacin, streptomycin, neomycin, kanamycin, gentamicin, paromomycin). Pregnancy: Do not use with pregnant women Lactating women: Tobramycin can pass into breast milk, so it should be used with caution, should only be used after consulting a doctor.
6. Drug interactions
Before the patient starts treatment with Brulamycin, it is necessary to inform the doctor about the drugs that he has been or is using recently to avoid causing drug interactions, reducing the effectiveness of treatment. or increase the side effects of Brulamycin. Some drug interactions of Brulamycin with other drugs are:
Muscle relaxants and diethylether may add to the neuromuscular blocking effects of tobramycin. Methoxyflurane when used as an inhalation anesthetic may exacerbate the nephrotoxic effects of injectable tobramycin. Amphotericin B, ciclosporin, cisplatin, vancomycin and furosemide: Increased side effects Avoid strong diuretics (ethacrynic acid, furosemide) as they increase risk of temporary or permanent hearing loss Acetaminophen, AcemetacinAbacavir, Aceclofenac: Types These drugs may decrease the rate of excretion of Tobramycin, which may lead to higher serum concentrations. Acenocoumarol: Increased risk or severity of bleeding reactions when Tobramycin is combined with Acenocoumarol. Acetylcholine: The therapeutic efficacy of Acetylcholine may be reduced when used in combination with Tobramycin. Acetyldigitoxin: The risk or severity of side effects may be increased when Tobramycin is combined with Acetyldigitoxin. Aminoglycoside: Concomitant use of Brulamyci with Aminoglycoside drugs has the potential to cause kidney damage. Brulamycin is an aminoglycoside antibiotic derived from Streptomyces tenebarius and is used to treat bacterial infections. To ensure the effectiveness of treatment and avoid unwanted side effects, patients need to strictly follow the instructions of the doctor, professional pharmacist.
Follow Vinmec International General Hospital website to get more health, nutrition and beauty information to protect the health of yourself and your loved ones in your family.