This is an automatically translated article.
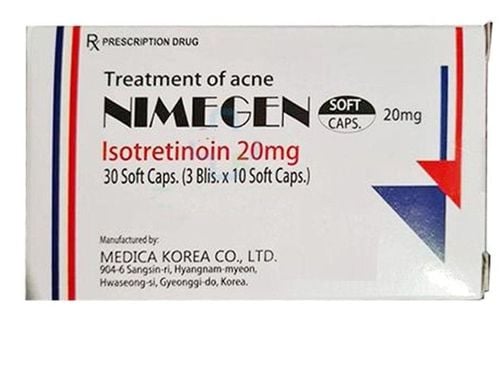
Acmolrine belongs to a group of dermatological drugs with isotretinoin as the main ingredient, which is used to treat severe forms of acne such as cystic acne, acne that is at risk of scarring after antibiotic resistance.1. What is Acmolrine?
Acmolrine medicine has the main ingredient isotretinoin that works to reduce sebum secretion and reduce sebaceous gland stimulation, thereby reducing scarring. In addition, isotretinoin also has anti-inflammatory properties. Acmolrine is usually prescribed in the following cases:Severe acne such as nodular acne, acne clusters. Acne with a risk of scarring has become resistant to antibiotics after systemic or topical treatment. Acmolrine is contraindicated in the following cases:
Pregnant and lactating women. Patients with liver failure. Patients with high blood lipids. Excess vitamin A. The patient is hypersensitive to isotretinoin or any of its ingredients. The patient is taking concomitant tetracycline antibiotics.
2. Dosage of Acmolrine
Acmolrine is usually used orally, during meals with doses depending on the subject and treatment goals:For adults, adolescents and the elderly:
Starting dose: 0.5 mg /kg/day. Adjust dose and duration of use depending on the patient, but usually 0.5-1 mg/kg/day will be used. With increases to 120-150mg/kg there is no significant additional benefit. A course of isotretinoin treatment usually lasts 16-24 weeks. If further treatment is required, it should be taken 8 weeks after the end of the first course of treatment. For special populations:
Patients with severe renal impairment: a lower dose (approximately 10 mg/day) should be started, which can be increased gradually up to 1 mg/kg/day or the maximum tolerated dose. Children: Isotretinoin should not be used in children under 12 years of age. Intolerant patients: For patients with intolerance to the recommended dose, it is advisable to start at a lower dose but for a longer duration of treatment but with a higher risk of relapse. When using isotretinoin overdose can manifest like an overdose of vitamin A: Headache, nausea, vomiting, drowsiness, irritation and itching, redness of the face, dry lips. These symptoms will subside without treatment. In addition, the concentration of isotretinoin in semen is higher than normal, so it is necessary to avoid sex with a pregnant or potentially pregnant woman for 1 month after overdose, and should not give blood for at least 1 month after the occurrence. isotretinoin overdose.
3. Acmolrine side effects
In some patients when using Acmolrine can experience side effects such as:Dry mucous membranes: dry lips, nasal mucosa, nosebleeds, eye conjunctivitis, dry skin. Anemia, increased erythrocyte sedimentation rate, thrombocytopenia. Muscle pain, joint pain, back pain (especially in young people). Hypertriglyceridemia, decreased high-density lipoprotein. Headache. Allergic skin reactions, hypersensitivity reactions, anaphylaxis. Depression, mood swings. Mental disorder, suicidal ideation. Benign intracranial hypertension, convulsions, somnolence. Cataracts, color blindness, decreased vision, keratitis, papilledema, photophobia. Hearing loss. Vascular inflammation. Tracheal spasm, hoarseness. Colitis, ileus, gastrointestinal bleeding, nausea, enteritis, pancreatitis. Glomerulonephritis . Increased granulation tissue formation, discomfort.
4. Be careful when using Acmolrine
Some general notes when using Acmolrine include:Acmolrine has the potential to cause teratogenicity, so it is necessary to inform the patient and apply contraceptive measures during drug treatment. Pregnancy should be checked before, during and after isotretinoin treatment. Patients should not donate blood during treatment and 1 month after stopping treatment because isotretinoin can be dangerous to the pregnant woman receiving blood. Acne may increase at the beginning of treatment but will subside as treatment continues, usually within 7-10 days. When using Acmolrine should avoid exposure to strong sunlight or UV rays. Sunscreen with SPF 15 or higher is recommended. Should avoid laser skin treatment or use of chemicals that are abrasive to the skin for 5-6 months after treatment with Acmolrine because it increases the risk of keloid scars or increases or decreases skin pigmentation on the treated skin. Avoid waxing for 6 months after isotretinoin treatment because of the risk of skin peeling. Isotretinoin should not be used with topical agents that have a scabbing and keratinolytic effect because of increased skin irritation. Patients should use a warm cream or ointment to keep the skin and lips warm from the start of isotretinoin treatment because the side effect of Acmolrine is often dry skin and lips. Liver enzymes should be checked before treatment, 1 month after treatment and every 3 months during treatment. Consider dose reduction or discontinuation of isotretinoin if clinical signs of elevated liver enzymes are present. Check blood lipids during treatment with Acmolrine, if triglyceride levels are too high or there are signs of pancreatitis, the drug must be discontinued. Patients with severe diarrhea should stop taking Acmolrine immediately. Patients with hereditary fructose intolerance should not take this medicine. Patients with diabetes, obesity, alcoholism, dyslipidemia need to be tested before treatment.
5. Common drug interactions with Acmolrine
Common drug interactions with Acmolrine include:Concomitant use of vitamin A with Acmolrine is not recommended due to the risk of developing vitamin A excess disorder Co-administration of Acmolrine with tetracyclines increases benign intracranial pressure. Concomitant use of Acmolrine with corticosteroids increases the risk of bone loss leading to osteoporosis. When oral contraceptives and Acmolrine are used together, they can make the use of oral contraceptives ineffective, so it is necessary to use 2 methods of contraception, including at least 1 basic method, Phenytoin has been reported. cause osteoporosis when used together with the drug Acmolrine.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.