This is an automatically translated article.
TB prevention is an early treatment for TB carriers who are completely healthy and normal. TB prevention drugs and TB treatment are the same, but still need to be aware of some problems when using.
1. What is TB prophylaxis?
TB prophylaxis also known as treatment for latent TB infection . This is an early treatment for normal, healthy people who carry TB germs in their bodies.
A person with latent TB actually has TB and is not capable of spreading it to others. When conducting tests (on the skin or in the blood) TB bacteria are present, but when examining sputum and secretions, they are not found.
TB prophylaxis has been practiced in many developed countries for a long time. The aim of preventive treatment is to destroy the dormant TB bacteria, to contribute to preventing their progression and to effectively prevent the disease.
2. Who needs TB preventive treatment?
The following people need TB preventive treatment:
Newborns and young children whose mothers have tuberculosis or are frequently exposed to the disease; People who have a weakened immune system or are taking medication that reduces the function of the immune system; People with diseases such as HIV , diabetes , kidney failure ... People with low weight , malnutrition ; People infected with TB in the past 2 years.
Những người bình thường mang vi trùng lao cần được điều trị dự phòng lao
3. How is TB preventive treatment?
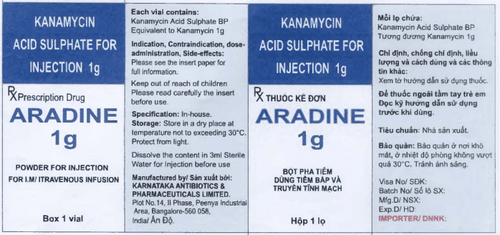
Preventative TB with drugs to reduce the risk of the bacteria progressing to TB in the future. TB prophylaxis and TB treatment are the same, but the duration of use is different. TB prophylaxis has a shorter duration.
There are 2 treatment regimens for latent TB infection, namely: Short-term and intermittent treatment.
Short-term treatment: Short-term TB prophylaxis is carried out over a period of 3 - 4 months with INH alone or in combination with rifampicin. This regimen is administered to TB carriers who are at high risk of developing TB disease and have a positive skin test. Intermittent Treatment: Intermittent TB prophylaxis also uses the drug INH at a dose of twice a week, performed on people working in the health sector, education or the homeless population. There are 2 ways to use TB drugs that patients can choose, that is, direct observation (DOT) and direct observation (DOT) treatment, specifically:
Treatment with DOT: Persons taking TB prevention treatment will be monitored and supported by staff and medical staff during the drug use process to ensure completion of the process. With this method, patients will be consulted, detected and treated side effects when taking drugs, if any. TB prophylaxis with DOT results in a higher treatment completion rate. Non-DOT Treatment: People on TB prophylaxis will receive medication for 1 week. It is important to ensure that the medication is taken at the right time and in the right dose to complete the treatment process. The following are the recommended TB prophylaxis regimens:
INH 300mg: 9 months of treatment in HIV-infected patients. Note that the 6-month treatment regimen is not applicable to children, people with HIV infection or fibrous lesions on X-ray. INH 900mg: Treatment with direct observation twice a week for 6 months or 9 months. Rifampicin 600mg: Indicated for people who are resistant to INH, the duration of treatment is 2 months or there is direct observation with a dose of 2 times / week for 2 - 3 months. PZA 1500 - 3000mg: Indicated for people infected with HIV but intolerant to rifampicin, the duration of treatment is 2 months.

Khuyến cáo người bệnh sử dụng thuốc dự phòng lao theo phác đồ điều trị của bác sĩ
4. Possible side effects when using anti-tuberculosis drugs
The use of anti-TB drugs can cause some unwanted side effects. Depending on each person's ability to respond to the drug, side effects may or may not be experienced, with levels that can be mild or severe.
Common but not dangerous side effects when using TB prophylaxis: Nausea, red urine (because Rifampicin is red, causing body fluids to turn red), digestive problems symptoms such as stomach pain, loose or hard stools, fever, itching, rash, joint pain swelling, numbness, tingling in hands and feet, headache, fatigue, weakness. The side effects caused by the use of anti-TB drugs are not dangerous and can be managed with simple methods, but they will cause discomfort and inconvenience in daily life for the patient. Rare serious side effects when using TB prophylaxis include: Yellow eyes (white part), stomach pain, nausea, vomiting, fatigue, weakness, generalized rash. When seeing these symptoms, the treatment person needs to go to the hospital for immediate examination.
5. Things to keep in mind when taking TB prevention drugs
Do not drink alcohol during TB prophylaxis because it can increase the risk of liver damage. The use of pain relievers during TB prophylaxis can also cause metabolic problems in the liver, so talk to your doctor before taking them. Your doctor may ask you to have blood tests done during TB prophylaxis to check how your liver is responding to the medicine. If an abnormality occurs, the prophylactic drug should be discontinued. It can take 2 to 4 weeks for the body to respond to TB preventive medicine. At that time, the side effects will subside and gradually disappear. In summary, people on TB prophylaxis need to pay attention to taking the medicine on time and at the right dose so that the treatment process is complete, highly effective, and helps prevent TB germs from progressing to disease in the future.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.