This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Tran Quoc Vinh - Emergency Doctor - Department of Resuscitation - Emergency - Vinmec Nha Trang International General HospitalMyocardial infarction is one of the leading cardiovascular diseases causing hospitalization and death today. The current updated diagnostic criteria for myocardial infarction help in early diagnosis of myocardial infarction, enabling patients to receive prompt and active treatment.
1. Distinguishing types of myocardial infarction
Acute coronary syndrome is a serious event of coronary artery disease, one of the leading causes of cardiovascular death. The mechanism of acute coronary syndrome is the instability of atherosclerotic plaques in the coronary arteries, which rupture. If the rupture is large and forms a massive clot that fills the entire lumen, it will lead to an acute ST-segment elevation myocardial infarction, also known as a transmural myocardial infarction. If the rupture is smaller and the clot formed has not completely occluded the coronary artery, it will cause non-ST-elevation myocardial infarction and stable angina.Non-ST-segment elevation myocardial infarction and unstable angina are collectively known as non-ST-elevation acute coronary syndromes. These two diseases have similar clinical and electrocardiographic symptoms. The difference is that non-ST-segment elevation myocardial infarction is found to have elevated myocardial biomarkers while stable angina does not.
Acute ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction differ in terms of diagnostic criteria, approach, timing factors, and treatment modality.

2. Diagnostic criteria for myocardial infarction without ST elevation
2.1. Clinical features 2.1.1. Patient characteristics Patients with myocardial infarction without ST-segment elevation usually have an older age, a higher prevalence of diabetes, hypertension, and dyslipidemia than patients with ST-segment elevation myocardial infarction. .2.1.2. Symptoms Patients will typically present with coronary-type chest pain. The pain usually occurs after exertion but can also occur at rest. The nature of the pain is tightness, squeezing behind the sternum, which can spread to the left shoulder, to the chin and both shoulders, usually lasting more than 20 minutes.
2.1.3. Clinical examination Although of little value in diagnosing the disease, clinical examination plays an important role in differential diagnosis (differentiating from diseases such as bronchitis, pericarditis, sternocostal arthritis, etc.). ..), assessment of risk factors, complications,...
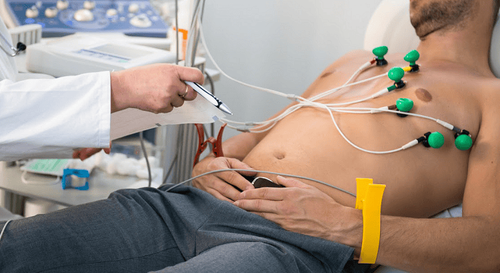
2.2. Subclinical 2.2.1. Electrocardiogram The most commonly seen electrocardiogram in chest pain muscle is ST depression, sharp T-negative, reversed, possibly transient ST elevation.
However, up to 20% of patients do not have an immediate change in the electrocardiogram, thus requiring repeated ECG measurements.
Electrocardiogram technique at Vinmec is carried out methodically and according to standard procedures by a team of highly skilled doctors and nurses, modern machinery system, thus giving accurate results, making a significant contribution to diagnosis and staging of the disease.
Cardiac biomarkers that can be used in the diagnosis and prognosis of acute coronary syndromes include: CK-MB. myoglobin, H-FABP, Troponins T and I. In which, Troponin T (TnT) and Troponin I (TnI) are two specific enzymes for the heart, when heart cells are damaged, these proteins will be released into the heart. blood. Troponin increases from the 3rd hour of infarct, peaks in 24-48 hours, and returns to normal after 7-10 days with Troponin I and 10-14 days with Troponin T.
Based on biomarker testing According to Troponin study, the two regimens currently used to diagnose non-ST-elevation acute coronary syndromes are the 1-hour regimen and the 3-hour regimen.
3-hour regimen to approach non-ST-segment elevation acute coronary syndrome based on changes in myocardial biomarker 1-hour regimen based on hs-cTn hypersensitive troponin test to diagnose myocardial infarction grade without ST-segment elevation or to rule out. 2.2.3. Echocardiography Echocardiography helps to evaluate left ventricular function, regional disturbances and concomitant valvular pathologies, and at the same time helps in differential diagnosis from other chest pain-causing diseases.
Vinmec International General Hospital is equipped with 4D ultrasound machine with modern features, high resolution, probe size, thickness, ability to pump blood, heart activities, .. Thanks to that, it helps to detect and diagnose abnormalities or complex pathologies of the heart in the most accurate way.
Along with the most modern ultrasound machine today is a system of facilities with a dedicated ultrasound room, computer software connected to the machine that allows accurate signal transmission. Especially, 4D ultrasound technique is performed by a team of professionally trained doctors, with absolute respect for technical rules. Therefore, the results obtained have very high accuracy, which is the basis for the doctor to give the best solution for the patient.

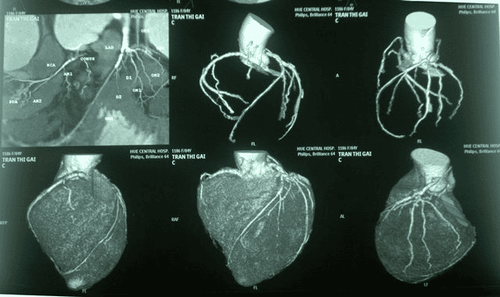
2.2.5. Coronary angiography Indicated in high-risk patients to perform coronary intervention if necessary..
3. Diagnostic criteria for acute myocardial infarction with ST elevation
3.1. Clinical features 3.1.1. Patient characteristics Patients at high risk for acute myocardial infarction with ST-segment elevation include those with unstable angina or multiple risk factors for coronary artery disease such as: overweight, obesity obesity, smoking, physical inactivity, stress, chronic diseases such as hypertension, diabetes, dyslipidemia. The disease usually appears in men over 45 years old and women over 55 years old, with a high frequency in the morning, from 6 am to 11 am, especially within the first 3 hours of waking up. In more than 50% of cases, patients have a trigger factor such as stress, exercise, severe medical illness, surgery.3.1.2. Physical symptoms Chest pain is the most common symptom, pain in the form of pressure, tightness, squeezing, pain behind the sternum or left chest pain, spreading to the neck, lower jaw, left shoulder or left ulnar border. In some cases, the pain may radiate down the epigastrium but never beyond the navel. The pain usually lasts more than 30 minutes and is accompanied by symptoms such as sweating and shortness of breath.
Some patients have no symptoms of chest pain but have other non-specific symptoms such as: fatigue, palpitations, dyspnea, nausea, vomiting, epigastric pain, altered consciousness,...

3.2. Subclinical To diagnose ST-segment elevation myocardial infarction, 3 tests should be performed as soon as the patient is suspected of having acute coronary syndrome: electrocardiogram, cardiac enzymes, and echocardiography.
3.2.1. Electrocardiogram should be performed immediately in the emergency room, should not be delayed more than 10 minutes.
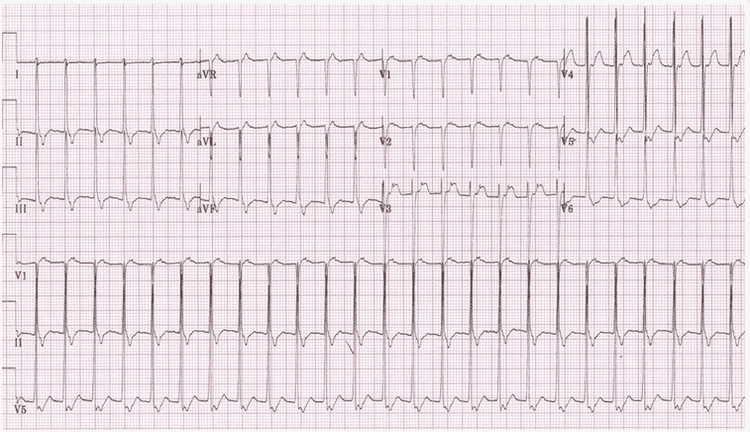
Acute complete occlusion of the coronary artery on the epicardium will produce ST elevation on the electrocardiogram. The majority of ST-segment elevation myocardial infarctions will progress to Q-wave infarction. ST-segment elevation and/or Q-wave leads help define the area of myocardial infarction. The contralateral radial leads of the infarct area will show ST depression.
Diagnostic criteria for myocardial infarction with ST-segment elevation on electrocardiogram are: J-point elevation in at least 2 consecutive leads: In leads V2 and V3 : Male <40 years old: J ≥ 2.5mm; Male ≥ 40 years old: J ≥ 2mm; Female : J ≥ 1.55 mm Other leads: J ≥ 1 mm Pathological Q wave criteria on electrocardiogram: At V2, V3: any Q life > 0.02 s or QS image In at least 2 consecutive leads have Q ≥ 0.03 sec and ≥ 1mm depth or QS image. At V1, V2: R>0.04 sec and R/S >1 with congruent positive T wave without associated conduction disturbances. Diagnostic criteria for myocardial infarction in patients with left bundle branch block or left ventricular pacing: Sgarbossa criteria, including: ST elevation in the same direction ≥ 1mm: 5 points ST depression in the opposite direction ≥ 1mm: 3 points ST retrograde elevation ≥ 5mm: 2 points If ≥ 3 points: diagnosis of myocardial infarction with 90% specificity. In patients with acute inferior MI, the right ventricular leads V3R to V6R should not be measured in order to determine if there is an associated right ventricular infarction. At V4R, if ST elevation ≥ 1mm helps to diagnose right ventricular myocardial infarction, however, this sign only persists in the first 10-12 hours of infarction.
Image of posterior myocardial infarction can be detected indirectly through mirror image at V1, V2, V3: R dominant (R/S > 1) and ST depression. Measure more V7. V8, V9 for definitive diagnosis: V7-V9 has ST elevation ≥ 0.5mm.
Infarct zoning on the electrocardiogram based on the ST-segment elevation lead is as follows:
3.2.2. Cardiac enzymes Troponin I and troponin T tests: to diagnose myocardial infarction at least one cardiac enzyme sample is elevated above the 99th percentile. If the first cardiac enzyme sample is negative, test the second sample after 4 -6 o'clock. If two troponins 4 to 6 hours apart are negative, acute myocardial infarction is excluded.
In cases where chest pain or ECG is not clear, hs Troponin (High Sensitivity Troponin) can be used. If the first test is negative, try again in 2-3 hours. The degree of elevation of Troponin correlates with the degree of myocardial mass necrosis.
CK-MB is a cardiac enzyme that increases 4-8 hours after an infarction and returns to normal after 48-72 hours. CK-MB is used to diagnose recurrent myocardial infarction during the subacute phase of myocardial infarction.
Cardiac enzyme testing is done for all patients in the acute phase but cardiac enzyme results should not be waited to initiate reperfusion therapy.

In addition to measuring 3 tests that need to be done immediately are electrocardiogram, heart enzyme test, echocardiogram, other tests such as kidney function, electrolytes, blood lipids and other routine tests such as complete blood count , whole blood coagulation,... should be performed within 24 hours of the patient's admission in order to comprehensively assess the patient's condition, as a basis for treatment methods.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors and a system of modern technological equipment. The hospital provides comprehensive, professional medical examination, consultation and treatment services, with a civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.