This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
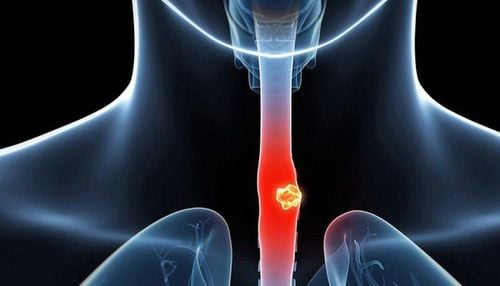
Esophageal cancer is a malignant lesion of cells originating from the esophagus, which can occur in any position of the esophagus, the disease is more common in men than women. The mortality rate from esophageal cancer ranks 8th among cancers in the world, the incidence rate varies from region to region. However, most diseases are related to smoking and alcohol consumption or nutritional habits and obesity.
5. The risk of developing esophageal cancer is higher in celiac disease
The risk of developing esophageal cancer is higher in celiac disease with an age-adjusted incidence of esophageal cancer of 50 per 100,000 person-years (normal 3.9). However, current data suggest that this risk is short-term, mainly within the first year of diagnosis. Achalasia has been linked to the development of esophageal cancer, although the risk is low. Brochure et al reported that esophageal cancer occurred in patients with achalasia at a rate 140 times higher than in the general population.
6. Esophageal adenocarcinoma
The main risk factor for adenocarcinoma is Barrett's esophagus (a hyperplastic change of the normally stratified squamous cells of the lower esophageal sphincter (eg, nitro-glycerin, esophagus). specialized columnar epithelial cells), anticholinergics, beta-agonists and benzodiazepines) and obesity in others. The increase in the risk of Barrett's esophagus and thus the growing obesity epidemic of adenocarcinoma parallels the increase in the absolute risk of Barrett's esophagus as the incidence of GERD and the increased incidence of adenocarcinoma. The rise of adenocarcinoma is controversial. As the only known premalignant lesion, the previously observed increase in the incidence of adenocarcinoma, it is recognized as a precursor of the majority of cases may have slowed down now. may be due to a change in adenocarcinoma with a 30-125 higher risk than in general during the natural progression of Barrett's disease or population growth. Risk of conversion from Barrett's esophagus to adenocarcinoma with exposure to protective factors. Aspirin and PPI use of 0.5% per year, and believed to occur up to 15 years, have been reported to reduce the risk of transition after diagnosis. Diagnosis and management of Barrett's esophagus to adenocarcinoma while drugs known to relax the lower esophageal sphincter (eg, nitro-glycerin, anticholinergics, beta-agonists, and benzodiazepines) increases the risk of Barrett's esophagus and therefore adenocarcinoma.
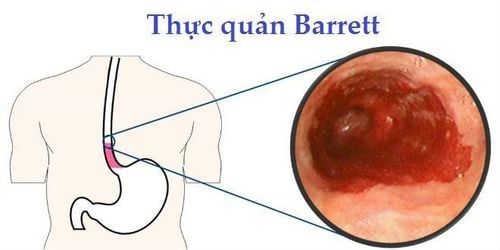
6. Barrett's esophagus and esophageal cancer
The absolute risk of adenocarcinoma in Barrett's is controversial. As the only known premalignant lesion, it is considered the antecedent of the majority of adenocarcinoma cases with a higher risk of 30-125 compared with the general population. The risk of conversion from Barrett's esophagus to adenocarcinoma is 0.5% per year and is thought to occur up to 15 years after diagnosis. The diagnosis and management of high-grade dysplasia (HGD) in patients with Barrett's esophagus is controversial. Lesions in a large number of patients with high-grade dysplasia may even regress or persist and not develop into cancer, providing the basis for recommendations for a less aggressive approach to management. Because Barrett's esophagus is a strong risk factor for adenocarcinoma, many advocates for endoscopic screening of patients with Barrett. However, the United States Agency for Disease Control and Prevention has not published any guidelines for or against screening for adenocarcinoma.
Previous studies have created an alarming picture of Barrett's esophagus and adenocarcinoma that seem to have been exaggerated. A systematic review of 47 studies found the overall incidence of Barrett's esophagus to be 6.1 cases per 1000 person years. The absolute risk of adenocarcinoma after a diagnosis of Barrett's esophagus was, in recent studies, several times, up to four to five times lower, than the risk reported in previous studies, form the basis for current monitoring guidelines. The risk of adenocarcinoma in patients with Barrett's esophagus may be so small that, in the absence of dysplasia, routine surveillance of these patients tends not to be recommended.
7. The role of PPIs in esophageal cancer
The impact of widespread use of Proton Pump Inhibitors (PPIs) on the increasing incidence of Barrett's esophagus is contradictory. PPI treatments offer a short-term benefit in symptom relief and healing of esophagitis, and possibly a long-term chemopreventive benefit in reducing the progression of dysplasia and cancer. High-dose PPI therapy for up to 5 years has mixed results and benefits. In a 13-year prospective study of 188 patients on PPIs, the incidence of adenocarcinoma was 0.31%, which is one of the lowest rates observed in real Barrett patients. management is monitored endoscopically. In contrast, PPI-treated patients with mild GERD symptoms or no GERD symptoms had a significantly higher incidence of adenocarcinoma compared with severe GERD symptoms.
8. Esophageal adenocarcinoma and obesity
The incidence of adenocarcinoma seems to parallel the increasing obesity epidemic since the mid-1970s. The increase in obesity accounting for 6.5% of the increase in adenocarcinoma occurred since 1973. to 2005 and 7.6% in 2005. The risk of obesity-related adenocarcinoma is higher in men than in women. The positive association between increased BMI and GERD in the United States was not consistently seen in other countries. Abdominal obesity appears to increase the risk of Barrett's esophagus, while waist-related obesity has a protective effect. Diabetes mellitus may be a risk factor for Barrett's esophagus, independent of obesity and other risk factors.

9. Helicobacter pylori (H. pylori) and esophageal cancer
Helicobacter pylori (H. pylori), a gram-negative bacteria, has been studied worldwide and in individuals of all ages in various diseases. Conservative estimates suggest that 50% of the world's population carry H pylori, mainly in developing countries where water and sanitation supplies are inadequate. H. pylori infection is a well-known risk factor for gastric malignancy with a risk up to 6 times that of the general population.
Recent advances in the treatment of H pylori, a gastric carcinogen, and its ability to effectively eradicate are considered one of the main reasons for the increase in esophageal cancer. Chronic H. pylori infection leads to atrophic gastritis, decreased acid production, and therefore a lower likelihood of severe GERD. H. pylori infection is associated with lower rates of Barrett and adenocarcinoma, especially the more virulent CagA-positive bacteria, which is associated with a higher frequency of gastric cancer.
Currently, Vinmec International General Hospital has implemented a package of screening and early detection of gastrointestinal cancers (esophagus - stomach - colon) Package of screening and early detection of gastrointestinal cancers (practice) esophagus - stomach - colon) of Vinmec combines clinical and paraclinical examination to bring about the most accurate results possible. Specifically, Vinmec's package of screening and early detection of gastrointestinal cancers (esophagus - stomach - colon) includes:
Gastroenterology specialist examination (by appointment) Gastroscopy and colonoscopy with NBI endoscope with anesthesia Gastroscopy and colonoscopy with anesthesia (Drugs) Gastroscopy and colonoscopy with anesthesia (VTTH) Routine histopathological examination fixed, transferred, cast , cut, stain... biopsies (upper gastrointestinal tract (esophagus, stomach, duodenum, papilla) through endoscopy Routine histopathological examination is fixed, transferred, cast, cut, stained. ..biopsy specimens (lower gastrointestinal tract through endoscopy (colon, rectum)
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Janeesh sekkath veedu , changing epidemiology of esophageal cancers worldwide – what do we learn? Epidemiology of gastrointestinal cancers,
2, practicalgastro, january 2014 • volume XXXVIII, issue 1. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. Mar-Apr 2005;55(2):74-108. Stavrou EP, McElroy HJ, Baker DF, Smith G, Bishop JF. Adenocarcinoma of the oesophagus: incidence and survival rates in New South Wales, 1972-2005. Med J Aust. Sep 21 2009;191(6):310-314.