This is an automatically translated article.
Post by Master, Specialist II Nguyen Thi Hoai Nam - Head of Pain Relief Unit - Department of Anesthesia and Surgery - Vinmec Central Park International General Hospital.
In breast surgery, nociceptive/inflammatory pain is caused by tissue damage, while neuropathic pain is the result of damage to the central and peripheral nerves, especially the intercostal nerves from the chest 2 to chest 6. Therefore, pain control is the primary goal of local anesthetic techniques in breast surgery.
1. Overview
Breast surgery is common among women. In 2020, it is estimated that there will be 276,480 new cases of invasive breast cancer and 80% of patients undergoing surgery in the US. In addition, plastic surgery breast augmentation or breast reduction is also increasing.
After breast surgery, the rate of acute pain accounted for 40%, vomiting and nausea also increased. This is the cause of prolonging hospital stay, increasing treatment costs, affecting surgical results as well as increasing the number of patients being re-hospitalized after surgery.
In breast surgery, nociceptive/inflammatory pain is caused by tissue damage, while neuropathic pain is the result of damage to central and peripheral nerves, especially the intercostal nerves from the chest. 2 to chest 6. Nerve pain usually begins immediately after surgery and can persist for many months. 50% of cases after breast surgery can lead to chronic pain, affecting quality of life, especially prolonged sleep disturbance. Inadequate pain relief was considered an independent risk factor. Pain control is the primary goal of anesthesia in breast surgery. Proper treatment of acute postoperative pain is essential to improve surgical outcomes and patient satisfaction.
For a long time, intravenous analgesia has been the main method for pain relief after surgery. The annual increase in the number of breast cancer and cosmetic surgeries has stimulated the development of new anesthetic techniques to improve pain relief and ensure safety, with fewer complications and side effects. .
2. Anesthesia trends and the role of regional anesthesia in pain management after breast surgery
International guidelines recommend multimodal analgesia in which PCA morphine plays an important role in analgesia after breast surgery. However, Morphine has many side effects such as itching, vomiting, nausea, respiratory failure, urinary retention, causing increased pain and persistent pain, which can progress to chronic pain after surgery. In addition, the rate of dependence and addiction on Morphine after breast surgery ranks third after total hip replacement and open cholecystectomy, so it becomes a burden to society and causes death due to drug overdose. Epidural anesthesia was once considered the gold standard in postoperative analgesia. Recently, many studies have shown that the benefits of epidurals are not as great as previously thought and the risks of the method have made it no longer the gold standard. The question is: “Methodology What is the safest and ideal method not only for immediate results after surgery but also for long-term results?”, where the important factors determining long-term outcomes are cancer recurrence. Chronic pain and the development of chronic pain.Current trends:General trend: Non-Opioid Anesthesia (Free Opioid Anesthesia & Analgesia) Ultrasound-guided Regional Anesthesia (Ultrsound-guided RAA) Over several decades In recent years, the benefits of peripheral nerve anaesthesia have been overwhelming, including improved clinical, economic, and humane benefits. The benefits of peripheral nerve anesthesia in multimodal analgesia These include:
Improved postoperative pain control and reduced use of Opioids Reduced length of hospital stay Prevention of re-hospitalization Reduce postoperative nausea and vomiting Faster transition to phase 2 resuscitation and/or skip post-anesthesia care unit (PACU Post Anesthesia Care Unit) Early physical therapy sessions Improve patient satisfaction Local anesthetic techniques can be performed as a single dose (single shot) either through a continuous infusion catheter or an intermittent auto bolus (intermittent auto bolus) before and after surgery. Local anesthetic techniques can be used alone or in combination with anesthesia in breast surgery, depending on the regional anesthetic method chosen. Meta-analyses showed that pain intensity 24-48 hours after surgery was significantly lower in the group of patients with combined regional anesthesia compared with the group receiving systemic morphine alone; At the same time, the amount of Morphine used was also less than the group that only used Morphine for the whole body.

In addition, side effects such as vomiting, nausea, itching, respiratory depression were also less common in the group with anesthesia. Studies have also shown that local anesthesia can prevent chronic pain. Some but not all experimental, animal, and retrospective clinical evidence indicates an association between anesthetic technique and cancer recurrence, but only prospective, randomized clinical trials can demonstrate a cause-and-effect relationship. These were patients with ongoing primary cancer randomized to receive 'anti-cancer' anesthesia (including regional anesthesia with propofol-based general anesthesia) or standard general anesthesia with reduced opioid pain and results are awaited, as this process will take another 3–7 years.
Risks and limitations of regional anesthesia:
Intravascular injection, bleeding Nerve damage Local Anesthetic Systematic Toxicity (LAST) Infection of the anesthetic site (more common in the catheter group) into the pleura causing pneumothorax.
3. Update and selection of local anesthetic techniques in breast surgery
Depending on the type of surgery, you can choose an anesthetic technique suitable for the purpose of anesthesia during surgery or analgesia after surgery. Regional anesthesia can be performed alone or in combination with sedation or general anesthesia.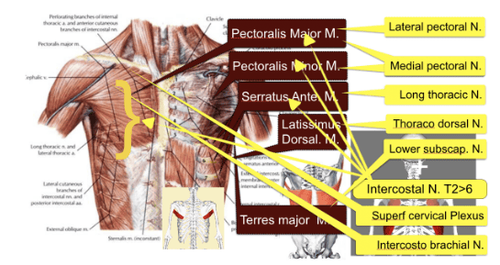
Thoracic epidural is no longer the method of choice because the risks outweigh the benefits as was previously thought.
Spinal edge numbness First performed in 1905, became a fairly popular method of postoperative pain relief in the early 20th century. However, it subsided after that and returned in 1979 after the article. by Eason and Wyatt is published. The technique of paravertebral anesthesia can be performed based on anatomical landmarks, but today subsonic anesthesia reduces complications and improves the success rate of the method. Local anesthetic is injected into the paraspinal space, acting on the spinal nerves and causing blockade of the corresponding region on the same side of the anesthetic. This is an easy technique to perform, reduces pain during and after surgery, prevents as well as treats chronic pain after surgery, stabilizes hemodynamics, does not cause paralysis of the limbs, reduces the risk of breast cancer recurrence. This is an alternative method of epidural anesthesia, single-dose injection or continuous infusion catheter, which can be combined with general anesthesia or sedation for surgery and postoperative pain relief. For mastectomy with or without axillary lymph node dissection, the numbing position is from C6-T6, in breast augmentation surgery T1-T6.
Spondylolysis (ESP) In 2016, Mauricio Forero reported the first 2 cases of vertebral plane anaesthesia for the successful treatment of chronic chest pain. Thereby opening up a new method of anesthesia that can be combined with general anesthesia in surgery of the chest and upper abdomen. The drug is injected into the intermuscular plane between the great filling muscle and the erector vertebral muscle. The ESP anesthetic site in breast surgery is T3. For breast augmentation, ESP single shot; In case of mastectomy with or without axillary lymph node dissection, ESP catheter maintains local anesthetic in Intermittent auto bolus mode.
PEC1 chest wall anesthesia: Method to numb the muscle between pectoralis major and pectoralis minor, block the external thoracic nerve, suitable for day surgery, can replace paraspinal and epidural anesthesia. Rafael Blanco performed on 50 patients with reconstructive surgery/breast cancer and implantation in 2 years.
PEC2: Method of intercostal anesthesia between pectoralis minor and anterior molar muscles, blockade of 3-6 intercostal nerves, brachial intercostal nerve and long thoracic nerve. Described by Rafael Blanco 2012 in the journal Rev Anestesiol Reaim, in combination with PEC 1 for pain relief in breast surgery.
Anterior tooth muscle plane numbness: Method of interfacial anesthesia between the anterior teeth and the broad dorsal muscle, blocking the intercostal nerve in the thoracic region, the thoracic dorsal nerve and the long thorax. Described in 2013 by Rafael Blanco and reported in 2016 by Rakhi Khemka in breast reconstruction surgery.
Intercostal neuralgia During breast augmentation surgery, use 5ml of Marcaine 0.25% with Adrenaline 1:400,000 for each intercostal nerve from T2-T6.
Incisional anesthesia and catheters Incisional anesthesia with Anaropine before skin incision or after surgery have similar analgesic results in mastectomy with axillary lymph node dissection.
Multihole catheter: Used since 1935, it is still a safe and effective method of postoperative pain relief through many improvements in design. The drug is administered continuously through a multi-hole catheter placed along the incision and connected to an Elastomeric auto-pump.
Liposomal Bupivacaine: Bupivacaine lasts 72 hours. Used for single-dose anesthesia for the trapezius interstitial, femoral nerve, transverse abdominal plane (TAP)... In October 2011, FDA approved the use of surgical infiltration anesthesia for hemorrhoidectomy and hemorrhoidectomy. cervical vertebrae cut. In December 2015, FDA approved wider use to numb the incision to relieve pain in thoracic, abdominal and orthopedic surgery. In breast reconstruction and breast augmentation, the dose of Liposomal Bupivacaine can be used up to 600mg. The analgesic effect can last 3-5 days. Note, do not use more anesthetic 96 hours after injection. However, the drug is still not widely used due to its high price compared to existing anesthetics.
Depending on the location and surgical method, it is possible to combine methods of local anesthesia to achieve the best pain relief for the patient. The possible combinations are:
Pec 1 + Pec 2 Thoracic paraspinal anesthesia + Pec 2 Thoracic paraspinal anesthesia + Anterior dentate fascial plane anesthesia thoracic ESP + Pec 2 thoracic ESP + Serratus Pec + incision catheter
4. Conclusion
The role of multimodal analgesia technique is increasingly developed, confirmed in the treatment of postoperative pain in general and breast surgery in particular. In which, the development and application of peripheral anesthesia in clinical practice is the task of anesthesia resuscitation. Under the guidance of ultrasound, the techniques of flat anesthesia, thoracic fascia have proved effective in the treatment of pain after breast surgery, consistent with the trend of non-Opioid Anesthesia (Free Opioid Anesthesia & Analgesia). to achieve the ultimate goal of Free Pain Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.