This is an automatically translated article.
Postpartum placenta, which occurs in about 1-3% of births, is a relatively common cause of obstetric pathology. This is usually diagnosed when the placenta cannot separate spontaneously during the third stage of labor when the patient is bleeding profusely in the event of placental abruption or if the placenta is confirmed. left over after most of the placenta is born spontaneously.
1. Overview of placental abruption
Residual placenta after vaginal delivery is diagnosed when the placenta is left in the uterine cavity. Normal delivery requires full uterine contractions, with shedding of the placenta from the uterine wall and expulsion of tissue. Therefore, placental retention can occur in cases of significant uterine atony, abnormal placental adhesions, such as placental accretion spectrum, or cervical closure prior to placental detachment.
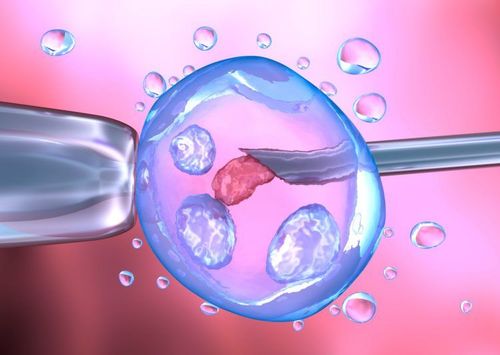
Risk factors for placental survival in parallel with uterine atony include prolonged oxytocin use, multiple births, preterm birth, history of uterine surgery, and IVF. A history of prior placental abruption and congenital uterine anomalies also appear to be risk factors.
Management requires manual removal of the placenta with appropriate analgesics, as medical intervention alone has not been shown to be effective. Complications may include major bleeding, endometritis, or retained portions of placental tissue, which can later lead to delayed bleeding or infection.
Prophylactic antibiotics may be considered for manual placental abruption, although evidence for efficacy is inconsistent. If bleeding is encountered, the initiation of a major transfusion procedure, aspiration with fluid aspiration, and the use of an intrauterine compression bandage, as with an intrauterine balloon, should be initiated immediately.
2. Risk factors
Many studies have attempted to identify risk factors for retained placenta. Established risk factors include anterior placental abruption, preterm birth, prior uterine surgery, previous termination of pregnancy, miscarriage or curettage, multiple births (greater than 5 previous births) and malformations. Congenital uterus (often undetected prenatally):
Risk factors associated with poor uterine contractility: Prolonged oxytocin use Risk factors associated with abnormal placenta: History uterine surgery, IVF conception Other risk factors: Prematurity, congenital uterine anomalies, history of previous placental remnants
3. Causes of placental retention after birth
The placenta can be retained if your contractions are not strong enough to push it out or if the cervix closes and keeps the placenta inside your uterus.
You are more at risk of having a placental abruption if you are over 30 years old, born prematurely, or if the first and second stages of labor are very long. It can also happen if you have fibroids or another problem with your uterus.
Many women will be given injections of syntocinon (a synthetic version of the hormone oxytocin), which will not only help supply the placenta but also help reduce the risk of postpartum bleeding.
4. What are the symptoms of a residual placenta?
The main symptom of placental abruption is that the placenta does not completely come out of the uterus after the baby is born. Another possible symptom is bleeding before the placenta comes off.
If part of the placenta is left behind, you may have symptoms a few days or weeks after giving birth. These may include:
Fever Bad-smelling discharge from the vagina Heavy bleeding Large pieces of tissue coming out of the vagina Pain
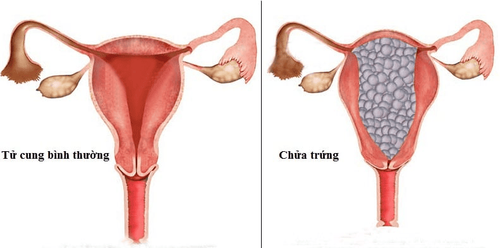
5. Diagnosis of missing vegetables through ultrasound images
Image of placenta left on ultrasound and along with it is a clinical examination when there are symptoms of abdominal pain, fever, vaginal bleeding a lot. Therefore, when mothers after giving birth have such abnormal symptoms, they need to go to a medical facility immediately so that the doctor can examine and determine the cause for timely handling. Because of the many potential risks that can endanger the lives of mothers.
For these reasons, the doctor will use ultrasound to see the damage and images of the placenta and take timely measures to avoid consequences such as hemorrhage, blood loss.
6. What is the treatment of placental abruption?
Sometimes a residual placenta can be treated simply if you empty your bladder, change position, and have your doctor or midwife gently pull the umbilical cord.
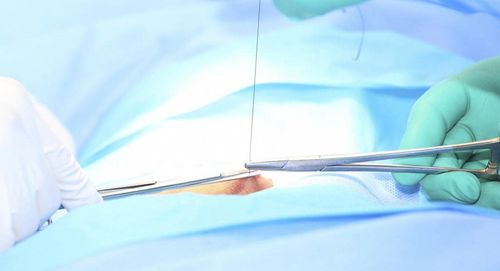
If that doesn't work, you will need a procedure to remove the placenta. You'll be put into surgery after birth and given an epidural or anesthetic so you won't feel anything. The doctor will use an instrument called a curettage to remove the lining of the uterus.
Pending surgery, the medical team will closely monitor you to check that you are not bleeding heavily (postpartum haemorrhage). This process is quick, but you'll need to be monitored for several hours afterward to make sure you're not bleeding.
If you start experiencing some of the symptoms mentioned above in the days and weeks after giving birth, it is important that you see your doctor immediately. It is not always clear after the placenta is born that some tissue may have been left behind and this can lead to infection and bleeding. If you have heavy bleeding after giving birth, you will need surgery to investigate the cause.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.