This is an automatically translated article.
Today, many young transgender people are using medical technologies to achieve gender transition. However, sex reassignment surgery can cause temporary or permanent infertility. As a result, many transgender people are now using technologies to preserve fertility. However, they may face dilemmas when making reproductive and family decisions, and face challenges in accessing and using fertility services.1. Research on reproductive methods for transgender people
Several studies done with transgender men in Belgium showed that 54% wanted to have children and 37.5% would consider freezing their eggs if this service was available. Many regret the missed opportunity for parents to have a genetically related child, and 77% think sperm conservation should be routinely offered to all transgender women.
Below is some information on fertility options for transgender people interested in hormone therapy or surgery compiled by Rainbow Health Ontario. Understanding and discussing reproductive options is an essential component of the Informed Consent Form for transgender-related healthcare and transgender rights. .
Note on terminology: Although most health care providers assume that all people with ovaries and uterus will be women and all people with testes and sperm will are male, so the community of completely transgender people (who have had their uterus, ovaries and testicles completely removed) is not the case for artificial insemination. In this article, transgender men are defined as those with ovaries and uterus or those with internal reproductive organs and transgender women as those who can produce sperm or those with reproductive organs. external genitalia.
2. Artificial insemination for transgender women
A transgender person who has testicles and plans to have them removed will need to have sperm removed before surgery to save sperm for later if he wants to have her own biological children. The World Professional Association for Transgender Health recommends that transgender women store their sperm at a sperm bank before starting hormone therapy to transition.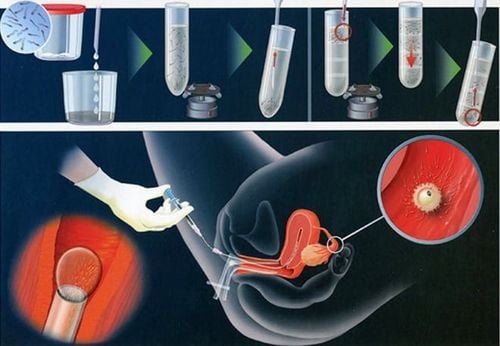
Thụ tinh nhân tạo cho nữ chuyển giới
Testicular volume is significantly reduced due to long-term estrogen use and affects sperm maturation and motility. Therefore, transgender women are better off storing sperm before using hormonal drugs. After surgery, transgender women cannot become pregnant because they do not have ovaries and uterus, so if they want to have children, they need an egg donor and a surrogate. For transgender people who are already taking hormones, it is advisable to temporarily stop taking hormonal drugs for a few months so that the testicles can produce sperm and the quality of the sperm can recover for storage. Several studies examining the effects of high doses of estrogen have shown that testicular function can be restored if use is stopped. If transgender people cannot interrupt hormone treatment, poor quality semen can still be frozen for later use with the help of advanced assisted reproductive technologies. In case the testicle is not capable of producing sperm through ejaculation, the medical facility will be able to perform microsurgery to extract spermatozoa to help find the sperm hidden deep inside the testicle. .
3. Artificial insemination for transgender men
Research shows that long-term use of testosterone does not weaken the ovaries and does not affect the ability of eggs to mature. For transgender people who are interested in reducing their fertility after using testosterone or they plan to have a hysterectomy and oophorectomy, there are two options available to preserve fertility:
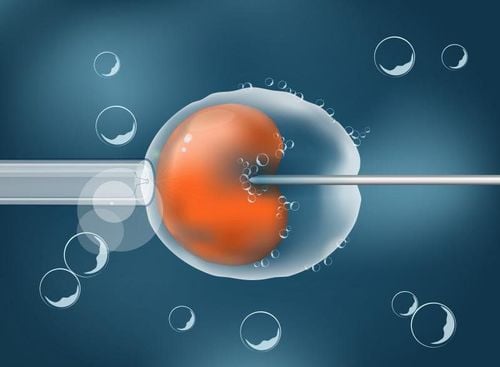
Bank oocyte delivery: By stimulating ovulation with hormones and removing the egg with a needle through the vaginal wall into the ovary, this technique is performed under ultrasound guidance. In some cases, frozen eggs do not survive because they are sensitive to the freezing and thawing processes. Embryo banking is taking eggs as above but will be fertilized immediately and put into the bank of embryos. This method will have a higher success rate than the above, but a sperm donor (whether anonymous or anonymous) must be selected at the time of egg collection. Freshly retrieved or stored eggs or embryos can be implanted in the original donor, in a partner's uterus, or in a surrogate.
Decisions regarding fertility preservation should be made as soon as possible. After the age of 30, ovarian tissue rarely has enough follicles for harvesting and cryopreservation. Transgender people who still have internal reproductive organs should consider performing embryo or egg freezing for better results before the age of 30
Recommended video:
How long after embryo transfer does the embryo implant?
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Articles refer to sources: ncbi, nhs, lgbtqhealth