This is an automatically translated article.
What is an abdominal aortic aneurysm and how to diagnose an abdominal aortic aneurysm early? These are questions that many people are interested in because it seriously affects health if not treated in time. The following article will focus on clarifying the role of ultrasound in the diagnosis of abdominal aortic aneurysm.
1. What is an abdominal aortic aneurysm?
The aorta is the large artery that leaves the heart and supplies blood to the body. It starts at the aortic valve that separates the left ventricle of the heart from the aorta and prevents blood from leaking back to the heart after a contraction, when the heart pumps blood. The different parts of the aorta are named based on their relationship to the heart and location in the body. Therefore, the beginning of the aorta is called the ascending aorta, followed by the arch of the aorta, then the descending aorta. The abdominal aorta extends from the diaphragm to the middle of the abdomen, where it splits into the iliac arteries that supply blood to the legs.
Abdominal aortic aneurysm is a focal dilatation of the abdominal aorta that is 50% larger than the proximal normal, or has a maximum diameter > 3 cm. (The aorta is a large blood vessel that supplies blood to the body). Because the aorta supplies blood to the body, ruptured aortic aneurysms can cause life-threatening bleeding. While you may never have symptoms, finding out you have an aortic aneurysm can be terrifying.
Most aortic aneurysms are small, unruptured, and slow-growing, but large aortic aneurysms can grow quickly. Depending on the size and rate of growth of the aortic aneurysm, treatment can vary from waiting to urgent surgery. Once an aortic aneurysm is found, the doctor will monitor it closely to proceed with surgery, which can be scheduled if necessary. Emergency surgery for a ruptured aneurysm can be fraught with risks.
Aortic aneurysms grow slowly and are often asymptomatic, making them difficult to detect. Some aneurysms will never burst. Many people start with a small and stable bulge, although it expands over time. Some aortic aneurysms slowly enlarge, growing less than 1.2 cm/year. Others expand at a faster rate, increasing the risk of dissection and rupture. The duration and extent of a dilated aortic aneurysm can be difficult to predict.
The most feared complication is aortic rupture, which is a surgical emergency due to its high mortality rate. Laboratory imaging has an important role in active surveillance.

Phình động mạch chủ bụng không bóc tách có thể biểu hiện như đau bụng dữ dội kèm theo đau lưng
2. Manifestations of abdominal aortic aneurysm like?
Nondissecting abdominal aortic aneurysm may present as severe abdominal pain accompanied by back pain. Non-dissection abdominal aortic aneurysm was defined as an aorta greater than 3 cm in diameter or greater than 50% dilatation of the aorta. Although risk factors for abdominal aortic aneurysm include tobacco use, male gender, and history of hypertension; A diastolic blood pressure above 100 mmHg is the most relevant risk factor for aneurysm formation.
In recent years, the worldwide incidence of nondissection abdominal aortic aneurysms has increased to 11%. Successful identification of an aortic aneurysm is critical in preventing the formation of aortic dissection, which accounts for 80% of mortality in patients with aortic aneurysms.
Mortality from ruptured abdominal aortic aneurysm is quite high: approximately 70% (range 59-83%) of patients die before hospitalization or surgery; for those undergoing surgical repair, mortality is ~40% and mortality after elective surgical intervention is 4-6%.
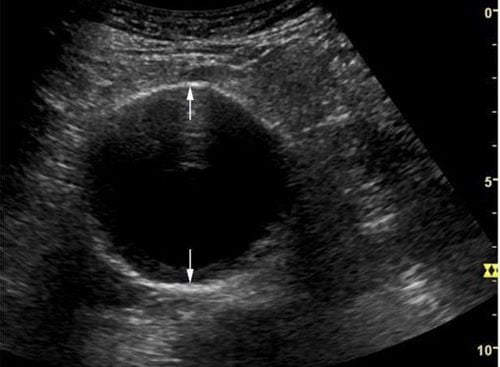
3. Ultrasound diagnosis of abdominal aortic aneurysm
Ultrasound is the optimal method for the examination and monitoring of abdominal aortic aneurysms in general, because it is rapid, eliminates the use of ionizing radiation and intravenous contrast, and is relatively inexpensive. 100% sensitivity and specificity approach; however, it should be noted that imaging is poor in 1% to 3% of patients due to patient habits or excessive intestinal gas.
Leaky or ruptured abdominal aortic aneurysm presents classically in patients over 60 years of age with a history of hypertension, atherosclerosis, and those with severe abdominal, back, or flank pain following an episode of syncope. Although abdominal aortic aneurysms are more common in men than women, the rate of rupture of membranes is higher in women because the growth rate of abdominal aortic aneurysms is significantly greater in women than in men.
Less than 50% of patients with ruptured abdominal aortic aneurysm present with the classic syncope triad, followed by lower back, lower flank or abdominal pain and a fluttering abdominal mass. Up to 30-60% of patients with abdominal aortic aneurysms are initially misdiagnosed. Therefore, the sonographer needs to be very careful not to confuse abdominal aortic aneurysm with more benign diagnoses such as renal colic, mechanical back pain, or appendicitis. Maintain a high index of suspicion in patients over 60 years of age presenting with abdominal, back, flank, or groin pain.
In addition, in patients at risk, urgent ultrasound can be a rapid and accurate method of identifying patients with abdominal aortic aneurysms who may benefit from follow-up or intervention. . The main disadvantage of ultrasound is that it can be difficult to distinguish a leaky or ruptured aneurysm from an enlarged but unruptured aneurysm. The aorta can also be difficult to visualize when the patient is obese or has bloating.
Siêu âm phình động mạch chủ bụng khi nghi ngờ phình động mạch chủ bụng
The abdominal aorta is said to have an aneurysm when the distal aorta is dilated to a diameter greater than 3 cm. An abdominal aortic aneurysm usually expands at a rate of 2-8 mm/y. Because enlargement leads to an increasing rate of rupture (eg, a 7cm abdominal aortic aneurysm has a rupture rate of 19-32% per year) and because the mortality rate with elective repair is much lower than with repair. For emergency treatment (3-5% vs 50%), the general recommendation is that abdominal aortic aneurysms larger than 5.0-5.5 cm should be electively repaired.
Although excellent for posterior lesions, ultrasound does not provide enough detail to plan procedures or more complex lesions. With a reported range in measurement error of 4mm12, ultrasound cannot reliably be used to evaluate endovascular treatments and evaluate regional branch vessels.
Doctors will order ultrasound in abdominal aortic aneurysms in the following cases:
Suspected abdominal aortic aneurysm As a diagnostic aid in the evaluation of patients over 60 years of age presenting with pain nonspecific dorsal, flank, abdominal, or inguinal For rapid evaluation of an unstable patient in the emergency or other acute care patient. The U.S. The United States Preventive Services Task Force (USPSTF) recommends:
Screening for abdominal aortic aneurysms once by ultrasound in men 65-75 years of age who have ever smoked. Selective screening for abdominal aortic aneurysms in men aged 65-75 years who have never smoked. Current evidence is insufficient to assess the balance of benefits and harms of screening for abdominal aortic aneurysms in women 65-75 years of age who have ever smoked. It is recommended against routine abdominal aortic aneurysm screening in women who have never smoked. In the appropriate clinical setting, ultrasonography alone can confirm the diagnosis of rupture when rupture occurs. However, if adequate images cannot be obtained (eg, due to obesity or flatulence) the diagnosis of aortic rupture cannot be ruled out.
Common mistakes when performing bedside ultrasound to evaluate abdominal aortic aneurysms include:
Failure to compress the lower bowel adequately with transducer pressure Mistaking the vena cava for the aorta due to pulses transmitted via Overestimation of aneurysm width due to lack of a true transverse measurement (cross section) Confusing imaging artifact with thrombus Failure to measure external diameter (from lateral wall to lateral wall) Failure to move transducer displacement from sagittal plane when monitoring aorta tortuous misinterpretation of distant enhanced aortic sound as evidence of leak. (Keep in mind that ultrasonography is not good at detecting ruptures or leaks. Contrast computed tomography – CT Scanner is the diagnostic criterion. However, contrast-enhanced ultrasound can be a useful diagnostic tool.) reasonable alternative to CT, if CT is not available) Do not want to move the transducer to the side to try to visualize an aorta obscured by enclosing intestinal gas.

Khuyến nghị can thiệp đối với phình động mạch chủ bụng ≥5,4 cm
4. Indicators to track
Some small aneurysms appear to be unchanged, while others slowly expand and are at risk of rupture. Regarding imaging, there is still debate about the best criteria for predicting ruptured abdominal aortic aneurysm and thus the indication for surgical intervention. Prognostic imaging criteria include:
Maximum transverse diameter The most widely used and validated method The Society of Vascular Surgery 2018 recommendations generally recommend intervention for abdominal aortic aneurysms ≥ 5.4 cm, and monitor lesions less than 19 in diameter. Young, healthy patients (especially female) may benefit from intervention for lesions 5.0 - 5, 4 cm.
Symptomatic lesions
In patients with connective tissue disorders (eg, Marfan syndrome), especially those with mitral regurgitation, immediate surgical treatment may be considered. even if the diameter is less than 5.0 cm.
Recommended imaging follow-up intervals for sub-adrenal aortic aneurysms vary by institution. American College of Radiology (2013) recommends:
< 2.5 cm: no follow-up 2.5-2.9 cm: 5-year interval 3.0-3.4 cm: 3-year interval year 3.5-3.9 cm: interval of 2 years 4.0-4.4 cm: interval of 1 year 4.5-4.9 cm: interval of 6 months 5.0-5.5 cm : Distance 3-6 months > 5.5 cm: treatment Society of Vascular Surgery (2018) recommends:
> 2.5-2.9 cm: Re-examination after 10 years 3.0-3.9 cm: Re-examination after 3 years 4.0-4.9 cm: Re-examination after 1 year 5.0-5.4 cm: Re-examination after 6 months Ultrasound is a non-traumatic, low-cost imaging method and can be performed many times compared with other imaging methods such as CT..., moreover, ultrasound has the ability to perform quickly in all medical facilities, potentially contributing to enhanced Accurate diagnosis rate in abdominal aortic aneurysm.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.













