This is an automatically translated article.
The article is professionally consulted by Master, Doctor Phan Ngoc Toan - Emergency Medicine Doctor - Emergency Department - Vinmec Danang International Hospital.Septic shock is a shock phenomenon when the body is severely inflamed, turning to sepsis, causing cardiovascular dysfunction. If not detected early and treated promptly, septic shock can endanger the patient's life.
1. Overview
1.1 Definitions
New definition according to SEPSIS-3, includes:Disruptive systemic inflammatory response syndrome to infection (sepsis): is a life-threatening organ dysfunction caused by ataxia body's response to infection. Identify: qSOFA≥2 or SOFA ≥ 2 points Septic shock: is a stage of sepsis in which severe circulatory and cellular metabolic abnormalities increase mortality. pulse + fluid replacement GOAL: • MAP≥ 65 mmHg
• Lactate 2 mmol/l
1.2 Tests to do
Specimens for bacteria:Get samples for testing early, preferably before antibiotics. Collect at least 2 blood samples to send for blood culture: At least 1 blood sample taken by peripheral venipuncture, one blood sample taken through each vascular access route has been stored for > 48 hours Sputum or bronchial fluid, cerebrospinal fluid urine, stool... Other tests: complete blood count, baseline coagulation, kidney function, liver, arterial blood gas, arterial blood lactate, procalcitonin...
Tests and probes help to detect present lesions, infection foci: Abdominal ultrasound, chest x-ray...

2. Treatment of septic shock
2.1. Initial Resuscitation (Hour-1 bundle “SSS 2016)
Targeted early treatment and carried out right at the emergency department, serious disease prevention:Blood lactate ≥2 mmol/l Blood culture right before using antibiotics (+/- RT-PCR Covid test) Antibiotic phone broad spectrum (+/- COViD-19 killer) Start crystalloid infusion of 30ml/kg if BP is low or Lactate is >1 mmol/l Immediate vasopressor if HS fluid is adequate and BP 65 mmHg Do not wait to enter ICU
2.2 Work packages Resuscitation continues for 6 hours
Use vasopressors (hypotension after fluid administration) to maintain BP >65, if in shock (Lactate ≥2 mmol/l or hypotension after adequate fluid resuscitation)SBP (8-12 mmHg) Oxygen saturation blood (make sure ScvO2 ≥ 70% or SvO2 ≥ 65 %) Urine flow ≥ 0.5mL/Kg/hour Re-measure blood lactate if initial lactate is high: If >4 mmol/l. Need to normalize lactate as quickly as possible
2.3. Control and maintain airway and breathing
Give enough oxygen to ensure SpO2 > 92% or no cyanosis. Consider early intubation and mechanical ventilation for patients with impaired consciousness, cyanosis or SpO2 that do not improve with oxygen, signs of respiratory muscle fatigue, or failure to restore hemodynamics.2.4 Restore circulation
Replenish salt crystals. Use vasopressors only when adequate fluid resuscitation is available. Not recommended: hydroxyethyl starches, gelatin, dextrans -1 Vasopressor options: First-line is norepinephrine, if +/- vasopressin is not available, Adrenaline Initial dose Noradrenalin 0.05 μg/kg/min increase dose by 0.05 μg every 5- 10 minutes if no response, maximum dose 5μg/kg/min. Add Dobutamine if unable to maintain ScvO2 ≥ 70% or SvO2 ≥ 65%. Initial dose is 3 μg/kg/min, increase to 3 - 5 μg after 5 - 10 minutes if no response, to a maximum of 20 μg/kg/min.
2.5 Antibiotics and infection control
Take specimens for bacterial testing before giving antibiotics. Intravenous antibiotics are recommended as soon as possible, within 1 hour, after the diagnoses of sepsis and septic shock have been made. In the treatment of COVID-19: applying antiretroviral regimens. If there is a bacterial or fungal infection, according to the causative organism, pay attention to multidrug-resistant hospital-acquired infections, especially in patients with hypoBC, secondary phagocytosis. It is recommended to use empiric broad-spectrum antibiotics, 1 or more antibiotics to cover all suspected organisms. If enterococci are suspected, add an antibiotic sensitive to enterococci such as vancomycin. Use broad-spectrum antibiotics according to de-escalation therapy Initial antibiotic: beta-lactam or 3rd, 4th generation cephalosporin May be combined with aminosides or quinolones Note: In patients with renal impairment, the dose of antibiotics must be based on creatinine clearance, the first dose should be used as usual, no dose adjustment is necessary, only the following doses should be adjusted..

2.6 Using Hydrocortisone
Only used when septic shock is poorly responsive to vasopressors or vasopressors have not been removed after 48 hours, caution is not used systematically.Dosage: 50mg every 6 hours (200mg/24 hours).
Reduce dose and stop when the patient is out of shock and the vasopressor is removed.
Note that may make the infection worse and cause hyperglycemia.
2.7 Blood products
Platelet transfusion when:Platelets < 10,000/mm3 (10 x 109/l) in the absence of obvious bleeding. Platelets <20,000/mm3 (20 x 109/L) if the patient is at risk of bleeding. Platelet count should be ≥ 50,000/mm3 [50 x 109/L] during bleeding, surgery, or invasive procedure.
2.8 Control blood sugar
Control of capillary blood sugar with insulin.Capillary sugar ≥ 11mmol/l, intermittent fast insulin treatment or continuous intravenous infusion depending on the patient's hyperglycemia.
Maintain blood sugar from 7 - 9 mmol/l.
2.9 Bicarbonate treatment
Sodium bicarbonate therapy should not be used for the purpose of improving hemodynamics or reducing vasopressor requirements in patients with tissue hypoperfusion causing lactic acidosis with pH ≥7.15.2.10 Prophylactic treatment of complications
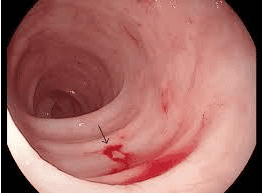
Venous Thrombosis: Low molecular weight heparin such as enoxaparin 1mg/kg subcutaneously, reduce dose in patients with renal impairment.Gastrointestinal bleeding: Use gastric mucosal drugs or proton pump inhibitors, note the route of administration and drug interactions.
The source of infection must be addressed by puncture, aspiration, drainage or surgery if indicated (must be done before continuous dialysis).
2.11 Measures to support organ function
Hemoabsorption (blood adsorption) combined with CRRT: therapeutic results may further support organ function.Adsorption. Elimination: TNF, IL, interleukin by HP
CVVH, CVVHDF techniques can be combined with IHD, HP, ECMO
-Do not choose to increase replacement fluid and dialysate to increase excretion of substances
-Increase progress membrane filter: adsorbs substances with large TLPT
Regarding membrane size (large area): 1.4-1.6 m2 High Kuf (increased ultrafiltration coefficient) New membrane technology and membrane material: membrane with high adsorption properties: oXiris (polymethyl methacrylate based on AN69 material); CytoSorb; Polymyxin B (PMX-B); PMX (TORAY Japan) well adsorbs cytokines.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.