This is an automatically translated article.
Abdominal pain, which can be acute or dull to spastic abdominal wall, is the main symptom of patients with acute peritonitis. Accordingly, initially, the pain may be dull and non-local, gradually progressing to severe and aggravated pain when there is any movement that causes the patient to strain. Therefore, understanding the mechanism of abdominal wall spasticity and early diagnosis of acute peritonitis has a great influence on the decision of the patient's condition.
1. What is acute peritonitis?
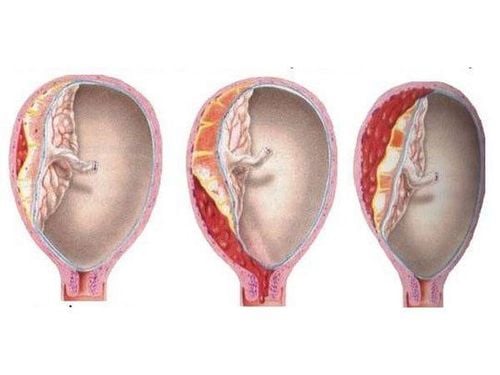
Acute peritonitis is defined as an acute progressive inflammation of the serosa lining the abdominal cavity and the organs it contains. Depending on the underlying pathology, the consequences of peritonitis can be infectious or aseptic (ie, chemical or mechanical). Whatever the cause, the abdomen is the second most common source of sepsis.
Acute peritonitis is usually caused by entry of infection into another sterile peritoneal environment through perforation of an organ but can also be caused by other irritants, such as foreign bodies, or bile from the gallbladder. perforated or ruptured liver or gastric acid from perforation of the gastrointestinal tract wall. Women also have focal peritonitis due to an infected fallopian tube or a ruptured ovarian cyst. Patients may have acute or insidious onset of symptoms, limited and mild initial illness, or rapid systemic progression, severe with septic shock.
The diagnosis of peritonitis is usually clinical. Diagnostic peritoneal lavage may be useful in patients who are unsuspicious on examination or who cannot provide a complete history. In terms of treatment, management for peritonitis and peritoneal abscess is based on systemic antibiotic therapy and supportive therapy to prevent or limit complications secondary to organ system failure. At the same time, early control of the source of infection is imperative and can be considered through non-surgical interventions including percutaneous drainage of the abscess, as well as percutaneous stenting and endoscopic surgery. However, in cases of acute peritonitis with severe intra-abdominal infection, emergency surgery may be required.
Viêm phúc mạc có thể gây tình trạng co cứng thành bụng
2. Characteristics of signs of abdominal wall spasticity in acute peritonitis
The diagnosis of peritonitis is usually clinical. The patient's history should take into account recent abdominal surgery, previous episodes of peritonitis, use of immunosuppressants, and the presence of intra-abdominal surgical disease (eg: inflammatory bowel disease, diverticulitis, peptic ulcer disease) increase the risk of infection.
Accordingly, the signs and symptoms commonly found in idiopathic bacterial peritonitis:
Fever and chills (up to 80% of patients) Abdominal pain or discomfort (present in 70% of patients) Patients) Worsening or unexplained encephalopathy Diarrhea Ascites that does not improve with diuretics Severe or new-onset renal failure Decreased intestinal motility Among which, abdominal pain, which may be acute or insidious, is the main complaint of patients with peritonitis. Initially, the pain may be dull and poorly localized - the mechanism is due to the new infection causing damage to the visceral peritoneum. Later, the pain became more stable, intense, and localized. This is an indication that the parietal peritoneum has also been affected. Even more, abdominal pain can be aggravated by any movement (eg, coughing, hip flexion) or any local pressure on the abdominal wall. This is the mechanism of abdominal wall contraction. If the underlying infection is not contained, the pain will spread. In certain pathologies (eg, gastric perforation, severe acute pancreatitis, intestinal ischemia), abdominal wall spasticity and peritoneal induction may be present at first.
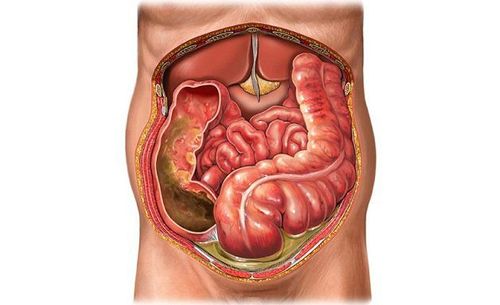
In addition to abdominal wall spasticity, patients with acute peritonitis examined may also note abdominal distension, as well as signs of dysfunction of other organs. Symptoms may be mild in patients receiving corticosteroids, diabetic patients with advanced neuropathy, and hospitalized patients, especially children and the elderly. In the presence of ascites, which is moderate to high volume of intra-abdominal fluid, the degree of friction between the viscera and the peritoneal surface is reduced, which can make the signs of peritoneal induction difficult to discern. Even the symptoms of abdominal pain in this group of patients became more vague than in patients without abdominal fluid.
In addition, anorexia and nausea are frequent symptoms and may herald the development of abdominal wall spasticity and peritoneal induction. Among these, vomiting can also be caused by underlying visceral disease (ie, a functional obstruction in the gastrointestinal tract) or secondary to irritation of the peritoneum when an inflammatory response occurs.

Co cứng thành bụng có thể khiến người bệnh buồn nôn và chán ăn
3. How to examine abdominal wall spasticity and peritoneal palpation
When examining a patient with peritonitis, the patient generally appears unwell and has acute abdominal pain requiring early hospitalization. While the majority of sick people have a temperature above 38°C, patients with severe sepsis can develop hypothermia. Tachycardia may be noted, due to release of inflammatory mediators, decreased intravascular volume due to anorexia, vomiting, and fever, as well as loss of third space into the peritoneal cavity causing ascites. With advanced dehydration and severe peritonitis, the patient may present in a state of critical septic shock.
When examining the abdomen of a patient with suspected peritonitis for signs of abdominal wall spasticity and peritoneal palpation, the patient should be placed in the supine position. At the same time, placing a soft blanket or pillow under the patient's knees so that the legs are slightly flexed, can help the abdominal muscles to relax better.
At this time, most of the patients have pain to palpation and will show increased abdominal wall stiffness depending on the level of abdominal pressure of the doctor. In particular, the increase in abdominal muscle tone can be spontaneous, termed spasticity, or to a certain depth when the abdomen is pressed, termed peritoneal induction.
In addition to physical examination, the characteristic of spasticity is reinforced by the observation that patients with severe peritonitis often avoid all movement and retain hip flexion to relieve abdominal wall tension. In addition, the abdominal wall is often observed to be distended and a reduced bowel sound is heard. These findings reflect functional bowel obstruction but may not be present if the infection is well localized in the first place. Occasionally, in addition to the characteristic abdominal wall spasticity, abdominal examination also reveals a focal inflammatory mass.
In a nutshell, peritonitis is an inflammation of the tissue that covers the organs in the abdomen, usually caused by bacteria. This is a life-threatening condition that requires urgent medical attention, especially when the patient is admitted to the hospital with an acute attack of abdominal pain and examination reveals signs of spasticity and peritoneal tenderness. Since a person with peritonitis can die within hours or days if not treated appropriately, this sign should be detected promptly through careful and thoughtful abdominal examinations.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.