This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Inflammatory bowel disease is a part of inflammatory bowel disease, Enteritis is a term used to describe general inflammation in the intestines caused by both bacteria and viruses. If inflammation occurs anywhere in the digestive tract, it disrupts the function of the organs, causing pain and life-threatening. Chronic inflammatory bowel disease includes two main diseases: ulcerative colitis and Crohn's disease.
1. Epidemiology
Joint involvement is the most common extra-gastrointestinal manifestation of inflammatory bowel disease, affecting 46% of patients. In addition to non-inflammatory joints with no actual swelling, which occurs in 8 to 30% of patients, arthritis of the spine (also called inflammatory disease of the bones of the spine) or peripheral joints has been well demonstrated. Initial reports classified peripheral arthropathy as either type I polyarticular (four or fewer peripheral joints) or class II polyarticular disease (five or more peripheral joints involved).
2. Overview of inflammatory bowel disease
Inflammatory bowel disease (IBD), which includes Crohn's disease and ulcerative colitis, are chronic autoimmune diseases of the gastrointestinal tract that affect more than 1.6 million Americans, with prevalence and prevalence worldwide. increasing demand. These diseases cause significant morbidity, frequent hospitalization, surgery, and use of corticosteroids and immunosuppressants. The annual direct and indirect health care costs of inflammatory bowel disease are estimated at $14.6-31.6 billion, with more than 50% attributable to hospitalization-related costs.
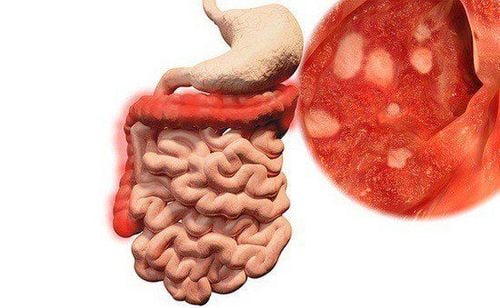
In addition to gastrointestinal symptoms and complications, inflammatory bowel disease is a systemic disease that is often accompanied by extra-gastrointestinal manifestations (extra-gastrointestinal manifestations) involving almost every organ in the body. . Extrasystoles may add to the adverse impact that inflammatory bowel disease has on affected patients in terms of pain severity, quality of life, and functional status.
3. Joint manifestations of inflammatory bowel disease
Among the extra-gastrointestinal manifestations of inflammatory bowel disease, those affecting the musculoskeletal system are among the most common, and have been reported in a number of series affecting 6 through 46% of patients. Idiopathic arthritis', which has been considered a disease group grouped under the heading 'degenerative spondylitis' (SpA), is also included in this category as psoriatic arthritis (psoriatic arthritis), ankylosing spondylitis ankylosing spondylitis (ankylosing spondylitis) and reactive arthritis.
Increasing understanding of the immunophysiology of these conditions, highlighting common changes in immune and inflammatory responses common to diseases with potentially diverse clinical manifestations . In addition, an increasing number of treatment options are available for patients with spondylolisthesis, with some agents being more or less effective for specific manifestations. Several agents used to treat spondylolisthesis have also been shown to be effective in inflammatory bowel disease, highlighting some of the common aspects of immunoregulatory dysregulation in these conditions.

4. Treatment
Arthritis can be functionally limited in patients with inflammatory bowel disease, so it should be noticed and treated in symptomatic patients.
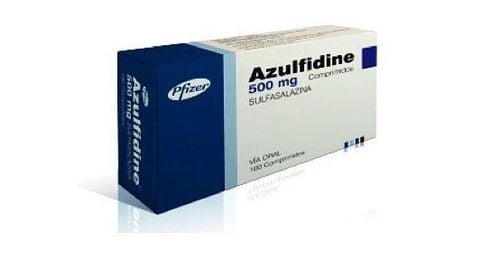
Much of the data regarding the treatment of peripheral arthritis associated with inflammatory bowel disease comes from the literature on the treatment of psoriatic arthritis (psoriatic arthritis) associated with peripheral arthritis. Treatment options include disease-modifying antirheumatic drugs (disease-modifying antirheumatic drugs), including methotrexate (MTX), sulfasalazine, leflunomide, and apremilast. Among biological agents, tumor necrosis factor (TNFi) inhibitors have the longest and largest clinical data supporting their significant efficacy. The most relevant data regarding the treatment of spondyloarthritis, also known as spondyloarthritis, come from studies of patients with ankylosing spondylitis.
5. Role of NSAIDs and cyclooxygenase 2 (COX2) inhibitors
While NSAIDs and specific cyclooxygenase 2 (COX2) inhibitors are effective in both peripheral and articular arthritis, their use in inflammatory bowel disease must take into account their potential effects on the gut. Short courses (less than two weeks) of NSAIDs, in particular, COX-2 inhibitors can be used for patients with inflammatory bowel disease.
However, caution should be exercised because NSAIDs can worsen underlying inflammatory bowel disease. In a large prospective cohort study of 791 inflammatory bowel disease patients in clinical remission at baseline, regular NSAID use ≥5 times per month was associated with a greater risk of Crohn's disease flare-ups, 7 times, but not ulcerative colitis; Less frequent use was not associated with an increased risk of inflammatory bowel disease exacerbations. In a meta-analysis of 7 studies involving 344 patients with inflammatory bowel disease, approximately 14.4% of patients treated with NSAIDs had worsening gastrointestinal symptoms.
6. The role of immunosuppressants
While disease-modifying anti-rheumatic drugs are not effective for spinal arthritis, TNFi is highly effective. IL-17 inhibitors, which have recently been shown to be effective in psoriatic arthritis and ankylosing spondylitis, would not be a good choice for inflammatory bowel disease-associated arthritis because they have may have an adverse effect on inflammatory bowel disease.

7. New strategies in the treatment of rheumatoid arthritis in patients with inflammatory bowel disease: a multidisciplinary approach to clinical integration with gastroenterology
Because of the significant overlap in inflammatory bowel disease and rheumatic diseases, the concept of a multidisciplinary approach in the combined gastroenterology-rheumatology clinical practice was explored. In a prospective study of 269 inflammatory bowel disease patients with arthralgia, Canigliaro et al observed that 50.5% of inflammatory bowel disease patients with arthralgia were diagnosed with inflammatory bowel disease. These patients had peripheral arthropathy in 53%, spinal arthropathy in 20.6%, and both peripheral and spinal arthropathy in 26.4% of patients. These patients have a higher incidence of other GI manifestations and are more likely to receive anti-TNF therapy than patients with inflammatory bowel disease without arthritis. The mean diagnostic delay was 5.2 years in these patients; however, with the establishment of a combined clinic, the delay in diagnosis has been greatly reduced.
8. Treatment of rheumatic complications in patients with inflammatory bowel disease
Extra-digestive manifestations and complications of rheumatic fever are common in patients with inflammatory bowel disease, presenting as peripheral arthritis and/or spondyloarthritis. These may or may not be related to inflammatory bowel disease activity, but can cause significant impairment in quality of life. A high index of suspicion and early treatment can reduce the healthcare burden.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Arthur Kavanaugh, Abha Goyal Singh, Rheumatologic Complications of Inflammatory Bowel Diseases, Dispatches from the guild conference, series
4, practicalgastro. Ott C, Schölmerich J. Extraintestinal expressions and complications in inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2013;10:585-95 Colia R, Corrado A, Cantatore FP. Rheumatologic and extraintestinal manifestations of inflammatory bowel diseases. Ann Med. 2016;48:577-58 Vavricka SR, Schoepfer A, Scharl M, et al. Extraintestinal Manifestations of Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:1982-92 Olivieri I, Cantini F, Castiglione F, et al. Italian Expert Panel on the management of patients with coexisting spondyloarthritis and inflammatory bowel disease. Autoimmun Rev. 2014;13:822-30 Molodecky NA, Soon IS, Rabi DM, et al. Increasing prevalence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2011;142:46-54