This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
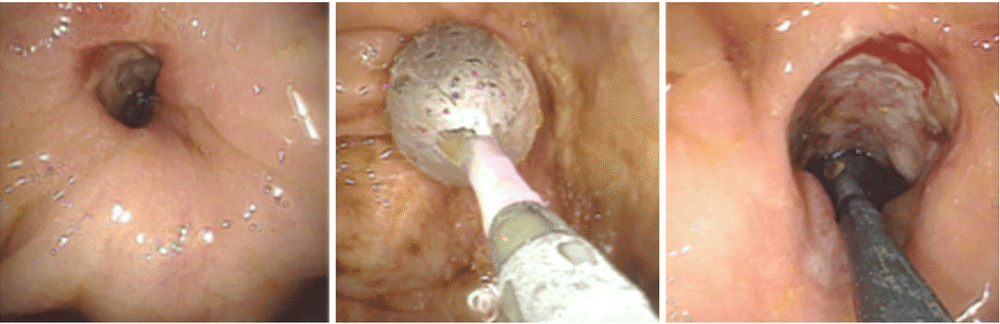
Regarding the therapeutic role of small bowel endoscopy in adult patients with complications of IBD, several studies have evaluated the clinical impact of endoscopic balloon dilation using an endoscopy system. Balloon-assisted enteroscopy for small bowel strictures in Crohn's disease.
Abbreviations:
Inflammatory bowel disease (IBD) Crohn's disease (Crohn's disease) Small bowel (SB) Capsule endoscopy (CE) DAE: assistive small bowel endoscopy; DBE: Dual Balloon Boweloscopy; SBE: Single-balloon endoscopy;
1. Therapeutic role of small bowel endoscopy in adult patients with complications of inflammatory bowel disease
Among them, Hirai et al., multi-author, the largest multicenter study to date conducted, enrolled 112 patients with symptoms of small bowel strictures associated with Crohn's disease to elucidate the efficacy and Safety of endoscopic balloon dilation technique. Ninety-five patients (85%) were enrolled, and balloon dilation was successful in 89 (94%) of them. The primary endpoint related to the short-term outcome was improvement in symptoms, achieved in 66 patients (70%). The dilation diameter was significantly larger (15.20 ± 1.70 mm vs 13.65 ± 2.59 mm, P = 0.03) in the short-term improvement group compared with the no improvement group. There were no other significant differences in baseline or small bowel stenosis characteristics of the groups.
2. Long-term results of endoscopic balloon dilation for small bowel strictures due to Crohn's disease
Long-term outcomes of endoscopic balloon dilation for small bowel stricture in adult patients with Crohn's disease have been extensively evaluated in two retrospective Japanese studies.
Hirai et al evaluated 65 Crohn's disease patients with symptoms of obstruction due to endoscopically manageable small bowel stricture (ligation length ≤ 5 cm, unrelated to fistula, pressure- car or deep ulcer and no severe curvature of ligation) with a clinical success rate of 80.0%. of the patient (52/65). During the follow-up period after the initial endoscopic balloon dilation (mean 41.8 ± 24.9 months), seventeen patients (26.2%) underwent surgery. Cumulative nonoperative rates were 79% and 73% at 2 and 3 years, respectively, and were significantly higher among successful laparoscopic balloon dilation (P < 0.0001). Furthermore, the cumulative non-renewable interest rate is 64% after 2 years and 47% after 3 years. No significant differences in concurrent therapy or initial balloon angioplasty were detected between patients with and without re-dilation.
More recently, Sunada et al analyzed data involving 85 patients undergoing endoscopic double-balloon-assisted endoscopic balloon dilation for SB-Crohn's disease and later were followed for a median of 41.9 months (range, 0-141). The non-surgical rate after initial endoscopic balloon dilation was 87.3% after 1 year, 78.1% after 3 years and 74.2% after 5 years. Univariate analysis showed that the presence of an internal fistula next to the refractory stenosis was significantly associated with the need for surgical intervention (hazard ratio: 5.50; 95% CI: 2, 16-14.0; P = 0.01).
3. Conclusion
Small bowel endoscopy appears to be a promising technique, especially in patients with suspected small bowel Crohn's disease alone and inconclusive results from routine diagnostic tests (including endoscopy). ileostomy and imaging studies such as CT Scan or abdominal MRI) where histological diagnosis will change the management of the patient. Furthermore, assistive small bowel endoscopy may have multiple roles for patients with known Crohn's disease, in terms of modifying medical therapy for deeper and longer lasting clinical improvement, Simultaneously diagnose and treat bleeding complications and pinpoint the exact location of the lesion to enable targeted surgical intervention.
As mucosal healing is increasingly the goal of Crohn's disease therapy, dual-balloon enteroscopy may have a role in assessing future response to therapy in most cases. determined. More standardized and broader studies are needed to confirm these evidences.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:Fong SC, Irving PM. Distinct management issues with Crohn's disease of the small intestine. Curr Opin Gastroenterol. 2015;31:92-97. [PubMed] [DOI] Sauer CG, Kugathasan S. Pediatric inflammatory bowel disease: highlighting pediatric differences in IBD. Med Clin North Am. 2010;94:35-52. [PubMed] [DOI] Hall B, Holleran G, McNamara D. Small bowel Crohn's disease: an emerging disease phenotype? Dig Dis. 2015;33:42-51. [PubMed] [DOI] Peyrin-Biroulet L, Loftus EV Jr, Colombel JF, Sandborn WJ. The natural history of adult Crohn's disease in population-based cohorts. AmJ Gastroenterol. 2010;105:289-297. [PubMed] [DOI] Pimentel M, Chang M, Chow EJ, Tabibzadeh S, Kirit-Kiriak V, Targan SR, Lin HC. Identification of a prodromal period in Crohn's disease but not ulcerative colitis. AmJ Gastroenterol. 2000;95:3458-3462. [PubMed] [DOI] Giovanni Di Nardo, Gianluca Esposito et al., Enteroscopy in children and adults with inflammatory bowel disease, World J Gastroenterol. Oct 21, 2020; 26(39): 5944-5958














