This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Rheumatic manifestations are the most common extraintestinal complications in patients with inflammatory bowel disease (IBD), and have been reported to occur in 6-46% of patients with IBD.
1. Joint manifestations of inflammatory bowel disease
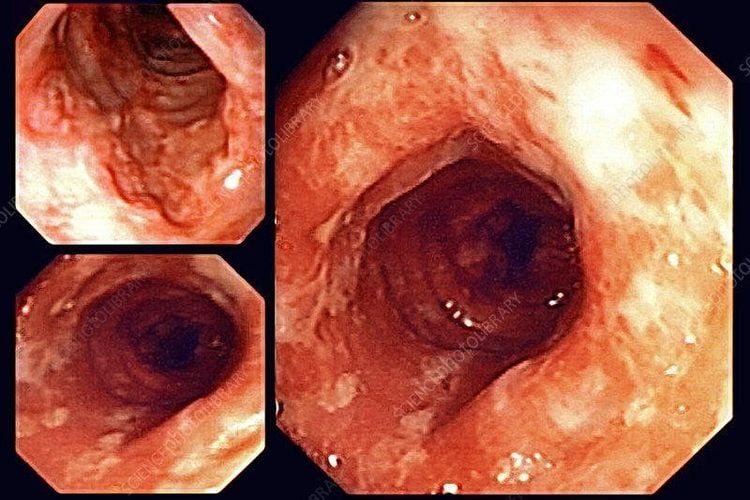
In addition to gastrointestinal symptoms and complications, inflammatory bowel disease is a systemic disease that is often accompanied by extra-intestinal manifestations (EIM) involving almost every organ system in the body. Common rheumatic extra-digestive manifestations and complications, presenting as peripheral arthritis and/or spondyloarthritis may add to the adverse impact that inflammatory bowel disease has on affected patients on pain, quality of life and functional status. Here we discuss the importance of a high index of suspicion and early treatment, which can reduce healthcare burden.
Rheumatic manifestations are the most common extraintestinal complications in patients with inflammatory bowel disease (IBD), and have been reported to occur in 6-46% of patients with IBD. Immunophysiology may be involved in the transport of abnormal lymphocytes from the inflamed intestine into the synovial bursa as well as extra-articular tissues, especially connective tissues. There are many potential clinical manifestations including peripheral arthritis, spinal or spinal arthritis, and inflammatory bowel disease. Peripheral arthritis associated with inflammatory bowel disease may be microarticular or polyarticular, with the former occurring earlier in the course of the disease, and sometimes transitioning to the latter. Much of the data regarding the treatment of IBD-associated peripheral arthritis comes from the literature on the treatment of psoriatic arthritis (PsA) associated with peripheral arthritis.

2. Does inflammatory bowel disease often cause joint manifestations?
Joint involvement is the most common extra-intestinal manifestation of inflammatory bowel disease, affecting 46% of patients. In addition to non-inflammatory joints with no actual swelling, which occurs in 8 to 30% of patients, arthritis of the spine (also called inflammatory disease of the bones of the spine) or peripheral joints has been well demonstrated. Initial reports classified peripheral arthropathy as either type I polyarticular (four or fewer peripheral joints) or class II polyarticular disease (five or more peripheral joints involved). More recent studies have shown that patients may present early with fewer joints involved and over time progress to a polyploid phenotype. In addition to peripheral arthritis, patients may have spinal arthritis.3. Characteristics of joint pain in inflammatory bowel disease
These patients often present with inflammatory back pain, usually defined as pain occurring in a younger person (eg, less than 40 years of age), worse in the morning, improving with use, and responding clinically. available with non-steroidal anti-inflammatory drugs (NSAIDs) therapy. Another area of inflammation common to spondylolisthesis is inflammation of the ligaments around the joints.
Periarticular tendonitis is inflammation of the areas where tendons, ligaments and joint capsule insert into bone. Inflammation in the ligaments around the joint is not only common, but may be an early aspect and may be implicated in the etiology of spondylolisthesis, including inflammatory bowel disease-associated arthritis. While musculoskeletal involvement often develops after the diagnosis of inflammatory bowel disease, in a small group of patients (<5%) joint symptoms may precede inflammatory bowel disease.
Risk factors for joint manifestations in patients with inflammatory bowel disease have been suggested to include a family history of inflammatory bowel disease, appendectomy, smoking, and the presence of extranodal manifestations. other digestive disorders such as erythema nodosum or pyoderma. Patients with generalized colitis (rather than proctitis alone) with Crohn's disease of the colon are thought to be more likely to develop extra-gastrointestinal manifestations in the joints.

4. Warning signs of inflammatory bowel disease with joint complications
As more effective therapies become available for the treatment of peripheral arthritis, spondylitis, and inflammatory bowel disease, early recognition becomes even more important. Some of the signs and symptoms that may be rapidly considered in association with musculoskeletal disorders in patients with inflammatory bowel disease include chronic back pain (eg, more than three months), peripheral joint pain and swelling, and cramping pain. and clavicle inflammation (full-digit swelling due to arthritis and multiple tenosynovitis)
5. Why can inflammatory bowel disease cause joint damage?
Rheumatic manifestations in patients with inflammatory bowel disease have been hypothesized to be due to activated intestinal lymphocytes in the joints and around the joints; These data suggest the presence of an 'enteric spine'. In patients with inflammatory bowel disease, lymphocytes of various subtypes can access joint sites using a variety of adhesion molecules and their antagonistic receptors. In addition to abnormal lymphocyte migration, dysbacteriosis, or altered gut microbiota diversity, there may be another common pathophysiological mechanism between inflammatory bowel disease and rheumatoid arthritis. related to inflammatory bowel disease.
6. Clinical Manifestations
Peripheral joint disease
Peripheral arthritis in inflammatory bowel disease often manifests as inflammatory arthritis, pain and swelling of the joints. Traditionally, inflammatory bowel disease-associated arthritis was generally considered non-corrosive and non-destructive; however, it is likely that these considerations are one-sided, and therefore may not be an accurate distinction.
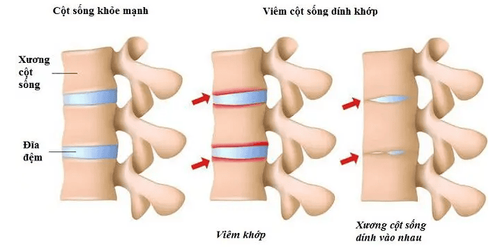
Arthritis of the body spine
Involvement of the spinal bones (bones of the body's spine) is a common feature of inflammatory bowel disease - arthritis. Typical symptoms are back pain caused by inflammation; Other features of ankylosing spondylitis have been well demonstrated in patients with inflammatory bowel disease-associated arthritis. These features are more commonly observed in patients with Crohn's disease (5-22%), compared with ulcerative colitis (2-6%).
7. Other rheumatic complications in inflammatory bowel disease
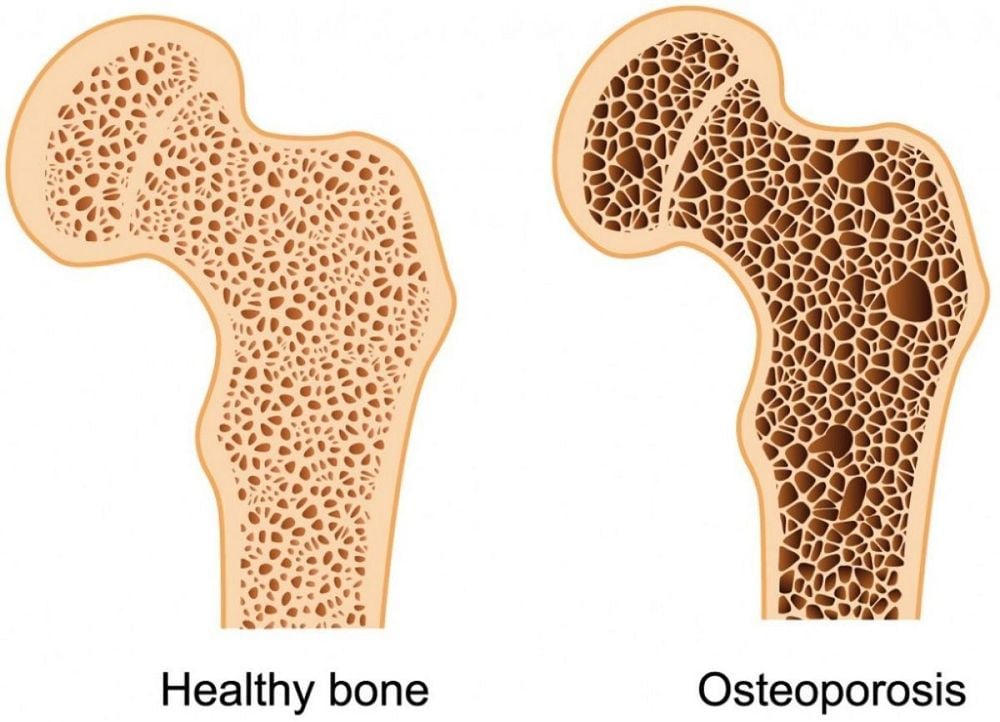
Although osteoporosis is probably not an extra-gastrointestinal manifestation of inflammatory bowel disease, it is indeed a commonly observed complication, occurring in approximately 14-42% of patients. It is multifactorial and is associated with several factors including intestinal malabsorption due to active disease or surgical resection, recurrent exposure to corticosteroids, and the local and systemic effects of systemic inflammation chronic. National guidelines recommend screening patients with inflammatory bowel disease for common risk factors for osteoporosis by dual-energy X-ray absorptiometry.
8. Conclusion
Extradigestive rheumatic manifestations and complications are common in patients with inflammatory bowel disease, presenting as peripheral arthritis and/or spondyloarthritis. These may or may not be related to inflammatory bowel disease activity, but can cause significant impairment in quality of life. A high index of suspicion and early treatment can reduce the healthcare burden.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Arthur Kavanaugh, Abha Goyal Singh, Rheumatologic Complications of Inflammatory Bowel Diseases, Dispatches from the guild conference, series
4, practicalgastro. Ott C, Schölmerich J. Extraintestinal expressions and complications in inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2013;10:585-95 Colia R, Corrado A, Cantatore FP. Rheumatologic and extraintestinal manifestations of inflammatory bowel diseases. Ann Med. 2016;48:577-58 Vavricka SR, Schoepfer A, Scharl M, et al. Extraintestinal Manifestations of Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:1982-92 Olivieri I, Cantini F, Castiglione F, et al. Italian Expert Panel on the management of patients with coexisting spondyloarthritis and inflammatory bowel disease. Autoimmun Rev. 2014;13:822-30 Molodecky NA, Soon IS, Rabi DM, et al. Increasing prevalence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2011;142:46-54