This is an automatically translated article.
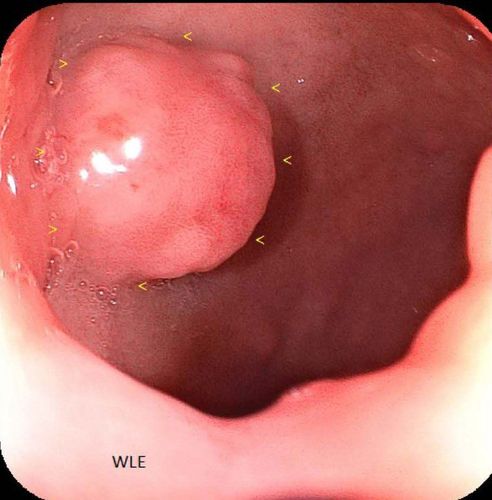
The article is written by Master - Doctor Mai Vien Phuong - Head of Gastrointestinal Endoscopy Unit - Department of Medical Examination and Internal Medicine - Vinmec Central Park International General Hospital.Mixed tumors of the colon and rectum, consisting of a combination of epithelial and endocrine factors with both benign and malignant potential, are rare neoplasms. These tumors can occur anywhere in the gastrointestinal tract and are often diagnosed incidentally. Given the rarity and marked heterogeneity of these mixed tumors of the colon and rectum with different histological phenotypes, establishing guidelines for optimal management strategies remains a challenge. challenge.
Abbreviation: MEEN: Mixed Endocrine Epithelial Tumor; MANEC: Mixed neuroendocrine adenocarcinoma; MANET: Mixed neuroendocrine adenoma; NET 1: Grade 1 neuroendocrine tumor; NET2: Grade 2 neuroendocrine tumor; NET3: Grade 3 neuroendocrine tumor; NEC: Neuroendocrine carcinoma. MiNEN: Mixed non-neuroendocrine neoplasm.
1. Optimal management strategy
Many cases of mixed endothelial carcinoma (MEEN) are locally advanced or may have synchronous metastases. Recurrence disease is also aggressive, develops at a rapid stage and metastasizes to many locations. Although both components can metastasize, the component is usually poorly differentiated.Nodal metastasis was detected in 72% of patients, 20% had distant metastases, while all cases presented with lymphatic invasion. The most commonly reported distant sites of metastasis are the liver, para-aortic lymph nodes, bone, and lung, followed by the peritoneum. Histological classification of the primary tumor is not an accurate predictor of metastatic pattern. As discussed previously, unusual patterns of metastasis from colorectal MEENs to the brain, meninges, or inguinal ganglia may occasionally be encountered. In the case of metastatic MEEN, treatment should target the components present in the metastasis, depending on their respective malignancy.
The optimal management strategy for patients with mixed endothelial neoplasms has not been determined due to their rarity. The majority of cases - up to 92.5% - are surgically removed with curative intent. Surgical resection of R0 with appropriate negative margins is targeted for localized disease with or without local involvement or locally advanced disease.
The surgical approach is adjusted depending on the location and extent of the disease. Often surgery can be performed to target both primary and metastatic lesions. Patients with manifestations of non-metastatic disease cannot perform surgical resection because the mortality rate does not allow. People with metastatic disease are evaluated on a case-by-case basis for the best treatment, surgery (done only 13.8% in palliative conditions) may not be the only option for most patients with metastatic disease.
In these patients, preoperative or adjuvant chemotherapy with or without radiation to surgically convert liver metastases, surgical dissection of the primary tumor, resection therapy, or targeted chemotherapy metastatic disease is used. Increasing physician awareness of the terminology and scope of MEENs/MiNENs plays an important part in optimal treatment decisions. Although the clinical presentation and surgical resection of MEENs/MiNENs are similar to those of adenocarcinoma alone, case-by-case recommendations should be discussed in a multimodal, both preoperative and postoperative manner for the complete management of the disease. present as soon as the diagnosis is confirmed.
2. Radiation therapy combined with chemotherapy
Radiation therapy combined with chemotherapy plays an important role in locally advanced or obvious lymph node involvement. These cases were treated with well-established preoperative protocols in the context of the multimodal tumor panel discussing and agreeing on the management plan for each case. Preoperative adjuvant irradiation is of particular importance for rectal lesions, with the primary aim of reducing bulky tumors for more efficient resection of the cancer, consistent with Gold standard in the treatment of rectal cancer to minimize local recurrence. There are no specific procedures specific to tumors with a mixed histology of epithelial and endocrine components.Role of chemotherapy: Nearly 40% of cases of gastro-pancreatic NEC (GEP) contain non-neuroendocrine components; including adenocarcinoma, signet ring cell carcinoma and, rarely, squamous cell carcinoma with WHO 30% resection criteria. In most cases of MiNEN, both the neuroendocrine and non-neuroendocrine components were poorly differentiated. The neuroendocrine component has proliferative indices in the same range as NEC but rarely one or both components can be well differentiated. The clinical manifestations of the disease largely depend on the neuroendocrine component of high-grade neuroendocrine tumors. The adenocarcinoma component affects the outcome only in cases where one of the two well-differentiated neuroendocrine components is present. MiNEN with well-differentiated neuroendocrine components should be considered as conventional rectal adenocarcinoma. While MiNEN with a poorly differentiated neuroendocrine component, the more common entity, should be considered a neuroendocrine carcinoma.

3. Full body treatment
Currently, prospective data are lacking to guide the authors in making treatment decisions for high-grade GEP NEC or MiNEN. If the neuroendocrine component is high-grade and poorly differentiated, current treatment recommendations are primarily based on retrospective data and extrapolation of data from small cell lung cancer (SCLC) because of the similarity in biological behavior.Patients with GEP NEC often have a poor prognosis with rapid disease progression. Multimodality therapy is recommended for most patients with early-stage disease/focal disease. These are chemotherapy-responsive tumors, and platinum chemotherapy is considered the backbone of treatment for both early and post-GEP NEC.
(1) Systemic treatment for localized disease: For early-stage disease, with potential for resection, surgical resection followed by 4 to 6 cycles of adjuvant platinum-based systemic therapy (cisplatin/carboplatin) plus etoposide is commonly used similar to the SCLC regimen.
The North American Society of Neuroendocrine Tumors (NANETS) recommendations recommend 4-6 cycles of adjuvant chemotherapy with platinum drugs (cisplatin/carboplatin) plus etoposide. Available data in limited-stage SCLC (small cell carcinoma) suggest that carboplatin and cisplatin are comparable in overall survival, progression-free survival, and client response rates. but with different toxicity profiles. Carboplatin causes many grade 3 – 4 hematological toxicities while cisplatin mainly causes neurotoxicity and nephrotoxicity.
Role of adjuvant radiation therapy:
Adjuvant radiation is reasonable if the risk of local recurrence is high, depending on the anatomical location of the tumor (eg, rectum). However, distant relapses are more frequent than local recurrences.
(2) Systemic treatment for metastatic disease: For metastatic disease, early palliative chemotherapy is essential due to the aggressive nature of high-grade neuroendocrine components. Standard chemotherapy consists of platinum plus etoposide.
In a retrospective study of Nordic GI NEC (upper gastrointestinal neuroendocrine carcinoma) patients, platinum plus etoposide was prescribed to 252 patients, 82/252 achieved complete remission . Median survival was 11 months in those receiving palliative chemotherapy compared with 1 month in 53 patients receiving the best supportive care. Response rates to initial chemotherapy were 31% and 33% when disease was stable. Those with Ki-67 <55% had a lower response rate (15% vs 42%) but better survival than patients with Ki-67 > 55% (14 vs 10 months). The most negative prognostic factors for survival were poor performance status, primary colorectal tumor, and elevated platelet or LDH levels.

4. Conclusion
Mixed endothelial neoplasms of the colon and rectum are rare, poorly understood entities that include a heterogeneous range of tumors with multiple combinations leading to tumors with high-grade malignant potential. , medium or low. This newly proposed revised term of mixed endothelial neoplasm will address the greatest barrier of confusion and misclassification that causes these rare types of colorectal cancer. Thus, it will facilitate the design of future multi-institutional randomized controlled clinical trials to develop and evaluate newer treatment strategies.Please follow the website: Vinmec.com regularly to update many other useful information.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Kanthan R, Tharmaradinam S, Asif T, Ahmed S, Kanthan SC. Mixed epithelial endocrine neoplasms of the colon and rectum – An evolution over time: A systematic review. World J Gastroenterol 2020; 26(34): 5181-5206 [PMID: 32982118 DOI: 10.3748/wjg.v26.i34.5181]