This is an automatically translated article.
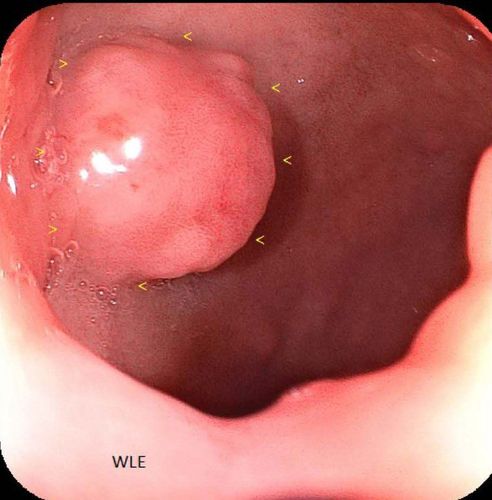
The article was written by Master - Doctor Mai Vien Phuong - Head of Gastrointestinal Endoscopy Unit - Department of Medical Examination and Internal Medicine - Vinmec Central Park International General Hospital.The term “mixed endocrine neoplasm” (MANEC) was coined by the World Health Organization in 2010 to refer to a type of cancer with a dual differentiation between adenocarcinoma and neuroendocrine carcinoma, each components represent at least 30% of tumors. In the following article, we will learn about the prognosis of this type of tumor.
Abbreviations in the article: MEEN: Mixed endocrine neoplasia; MANEC: Mixed neuroendocrine adenocarcinoma; MANET: Mixed neuroendocrine adenoma; NET1: Grade 1 neuroendocrine tumor; NET2: Grade 2 neuroendocrine tumor; NEC: Neuroendocrine Carcinoma; MiNEN: Mixed non-neuroendocrine neuroma.
1. Patients with mixed non-neuroendocrine neoplasms/mixed epithelial-endocrine tumors have a worse prognosis than well-differentiated NET1 and NET2 patients.
In the studies that investigated the prognosis of MiNENs/MEENs compared with other cancers, it was clearly found that patients diagnosed with MiNENs/MEENs had a worse prognosis than patients with NET1, NET2 alone. good domestication. However, it is still controversial whether MiNENs/MEENs have a better or worse prognosis than pure NECs. The biological behavior of MiNENs/MEENs is mainly driven by the endocrine component, of which, more than 90% of cases are poorly differentiated and, once metastatic, high-grade neuroendocrine carcinoma carries the prognosis. very bad and there is no definitive treatment option.
2. Prognosis of mixed neuroendocrine carcinoma
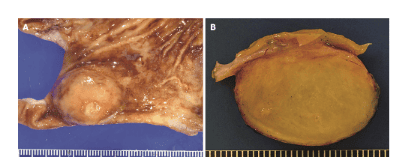
Compared with the survival rate of patients with adenocarcinoma, the survival rate of patients with MANEC is substantially worse. However, it is reported that the MANEC version of colorectal NEC appears less aggressive with the prognosis of pure colorectal NEC. Overall, the prognosis for MANEC remains poor with a median survival of 7-18 months from initial diagnosis, largely influenced by disease stage and tumor type.Better survival rates are noted in patients with localized disease than in patients with distant metastases. In another study, patients with colorectal MANEC and pure NEC showed similar survival. An Italian multicenter study of 51 patients with a diagnosis of high-grade MANEC of the gastrointestinal tract concluded that the prognosis of these tumors was primarily driven by the NEC component regardless of the type of treatment. what.
Most MANECs with a specific NET component in the large intestine are considered to be advanced disease, with deep invasion into the wall, lymph nodes, and distant metastases. However, recent recognition of unstable MANEC with a better prognosis than pure colorectal NEC is emerging as a unique clinical pathology subset of MANEC. Therefore, the prognosis of patients whose MANEC includes the NEC component needs to be better defined.
3. Factors contributing to the overall prognosis
There are many factors that contribute to the overall prognosis, headed by tumor size, histology, degree of differentiation, and then disease grade. The endocrine component is known for its rapid progression at diagnosis in the advanced stage, leading to poor survival as it appears to be responsible for the clinical course of the disease. Most studies lead to the conclusion that the degree of component differentiation affects the prognosis greater than the tumor volume.Gradually, the understanding of molecular mutations of prognostic significance is emerging with promise for targeted therapies. In this context, apart from somatostatin analogs, depending on KRAS status, a molecular predictor, the efficacy of anti-EGFR agents in mixed tumors unlike colorectal adenomas remains unclear. well known. Disease-free 5-year survival and overall 5-year survival were significantly lower in MANEC cases compared with those diagnosed with adenocarcinoma (60.5 % vs. with 76.2% and 69% vs. 82%).
4. Prognosis in stage IV disease
Specific prognostic factors or parameters not reported in the literature regarding survival of MANEC patients. However, MANECs with vascular invasion and CD117 expression at colorectal sites were reported to be independent prognostic factors, correlating with shorter survival.In contrast, large cell type, peritumoural lymphatic involvement, CD117(-), absence of vascular invasion, and methylation-induced microcytosis have shown an improved prognosis . In the cases of mixed non-neuroendocrine neuroendocrine tumors (MINENs)/Mixed epithelial-endocrine tumors (MEENs), no patient had a long-term survival of stage IV disease, with progression-free survival. The reported median progression was 4.5 months, while the median survival was 9.5 months, and no patient survived 17 months.
A higher volume of the high-grade neuroendocrine component (>50%) of the total volume of the tumor is thought to be an independent poor prognostic indicator indicating a lower survival rate. Adverse outcomes were associated with lack of chromogranin staining and strong somatostatin staining.
5. The most important prognostic factor
Overall, the most important prognostic factor reported was the overall Ki67 profile index in both components. The prognosis of moderate-grade MINENs/MEENs is usually determined by the non-neural epithelial endocrine component. Conversely, if there is a more aggressive neuroendocrine component such as poorly differentiated endocrine carcinoma, this automatically defaults to the predominant prognostic factor. It should be noted that both components can metastasize in an unpredictable fashion. However, low-grade MiNENs/MEENs mixed tumors including adenomas with well-differentiated low-grade neuroendocrine tumors have a relatively good prognosis and are considered a slow-progressing disease.Above is some information about the prognosis of mixed endocrine neoplasia of the colorectal. Please follow the website: Vinmec.com regularly to update many other useful information.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Kanthan R, Tharmaradinam S, Asif T, Ahmed S, Kanthan SC. Mixed epithelial endocrine neoplasms of the colon and rectum – An evolution over time: A systematic review. World J Gastroenterol 2020; 26(34): 5181-5206 [PMID: 32982118 DOI: 10.3748/wjg.v26.i34.5181]