This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Crohn's disease is an inflammatory bowel disease with symptoms of abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition. The inflammation caused by Crohn's disease often spreads deep into the layers of intestinal tissue, which is both painful and debilitating, and can sometimes lead to life-threatening complications.
Although there is no cure for Crohn's disease, care and treatment can significantly reduce the signs and symptoms of the disease and even bring about long-term remission.
1.Principles of treatment of Crohn's disease
For Crohn's, the choice of treatment modality depends on the location, severity, complications of the lesion as well as the patient's prognosis. The individualization of treatment is based on the degree of response demonstrated by symptom relief as well as the patient's tolerability. During the acute-onset phase, treatment to control symptoms to achieve “clinical remission” is necessary before entering the maintenance phase to stabilize the disease. When treatment to achieve remission, time can be from 2-4 weeks in most patients, however, in some cases, this period must last from 12-16 weeks. Patients who achieve a remission response will continue on maintenance therapy. Patients who are still symptomatic will have to choose another treatment modality.2.Evaluate the patient before treatment
Evaluation of patients in the acute phase will depend on clinical symptoms, mucosal lesions on imaging or endoscopic means, biomarkers such as CRP, fecal calprotectin. To facilitate the selection of treatment modality, Crohn's patients are usually divided into three groups: low-risk group with mild to moderate disease severity, high-risk group with disease severity from moderate to severe and the third group is the very heavy, ultimatum group.
Patients in the high-risk group include complications such as fistula, stricture, risk of intestinal obstruction, even intra-abdominal infection. Risk factors for severe progression include young age of onset, ileal involvement, multiple segment lesions, severe perianal or rectal disease, and fistula or stricture.
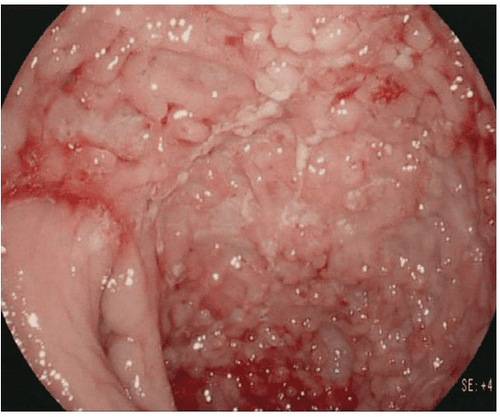
Low-risk group with mild to moderate disease activity: CDAI score of 150-220, usually responds to oral medications, and has no symptoms of dehydration, intoxication, pain, or presence Abdominal mass, intestinal obstruction, or weight loss >10% of body weight. The lesions on endoscopic examination of these patients are also not severe. High-risk group with moderate to severe disease activity: CDAI score from 220-450, not responding to treatment like low-risk group, often high fever, thin weight loss, abdominal pain, vomiting, nausea a lot (no evidence of bowel obstruction), severe anemia. The lesions on endoscopy range from moderate to severe. Very severe, fulminant group: CDAI score > 450, patients with persistent symptoms even after using corticosteroids or probiotics, presenting with high fever, persistent vomiting, evidence of intestinal obstruction or formation in an abscess or surgical sign. Endoscopic images show severe mucosal damage. The assessment of the severity of lesions on endoscopic examination is based on the scale of SES-CD, CDEIS presented in the section on endoscopic characteristics of Crohn's. During treatment, monitoring response and side effects is very important, especially when deciding to use biological products. When patients do not respond to this class of drugs, blood levels should be measured and antibodies to these biologics should be determined. Among the therapeutic drug groups, it is important to understand that some drugs with local action such as sulfasalazine, mesalamine, budesonide are broken down in the intestine while corticosteroids, mercaptopurine, azathioprine, methotrexate, biological products, cyclosporine A, tacrolimus have affects the entire gastrointestinal tract.

3.Treatment of fistula lesions and perianal pathology
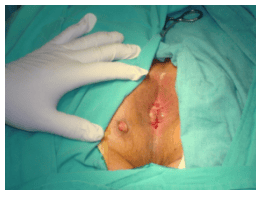
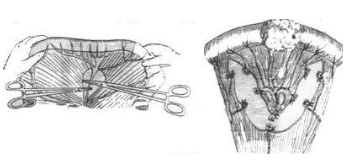
For patients with fistula lesions, the treatment needs to be closely coordinated between internal medicine and surgery. Fistula may occur in about one-third of patients with Crohn's, with perianal fistulas being the most common.Small, simple, and asymptomatic perianal fistulas do not require intervention. Symptomatic cases may only require the use of seton sutures to drain the fistula or may still require surgery. When evaluating for treatment options, it is possible to classify fistula lesions as simple (located far away from the fistula). dentate, single or complex fistula (multiple fistulas, located above, perforating or dilating the anal sphincter...).
Patients with no associated rectal mucosal lesions and simple fistulas may Respond well to surgery while patients with rectal mucosal lesions should consider drainage with seton thread rather than surgery
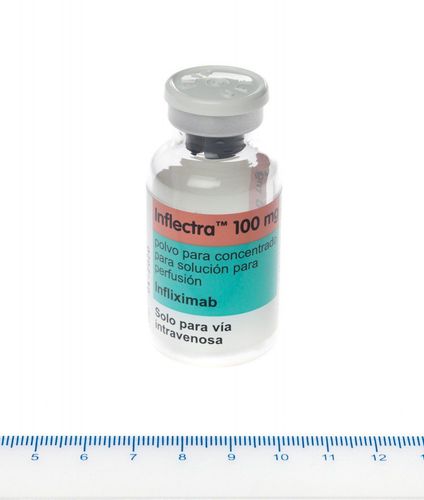
For medical treatment, the drugs infliximab, adalinumab, certolizumab pegol are recommended. Among these preparations, only infliximab has had randomized, controlled studies that confirm the healing effect of post-drainage fistula at the doses used as shown in Table 14. However, it should be noted that in this group of patients, before appointing the use of biological products, it is necessary to exclude lesions g abscess.
Small abscesses less than 5mm may not require drainage. Larger abscesses or complex fistulas require drainage to control inflammation and infection prior to biologics. The use of antibiotics such as metronidazole (10 - 20 mg/day, orally for 4 - 8 weeks) and/or ciprofloxacin 500 mg twice daily for 4 - 8 weeks) or levofloxacin (500 - 750 mg, once/day) for 4 to 8 weeks) improves symptoms and accelerates the healing of simple fistula lesions. In the cases of rectal, intestinal - bladder, intestinal - intestinal fistulas, it is necessary to use immunomodulatory drugs or anti-TNF group before surgery with the goal of resolving inflammation of the mucosa for intervention. surgery is favorable. In cases of fistula, drugs such as mesalamine or corticosteroids are often ineffective. Thiopurine drugs have been shown to be effective in this group of patients. Although tacrolimus can be effective in the short term, it has many unwanted effects, so it is not suitable for long-term use.
>> See more: Treatment of high-risk Crohn's patients - Article by Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital.
4. Maintenance treatment of Crohn's disease
For patients with no symptoms or very mild disease, maintenance therapy is not recommended. In patients with symptoms localized to a short bowel segment, surgery may be considered.
In patients who achieve remission following corticosteroid use, thiopurine or methotrexate should be considered. Steroid-dependent patients should be initiated early on immunomodulatory agents with or without anti-TNF contraindications.
According to the recommendations of the American Gastroenterology Association in 2018, do not use 5-ASA corticosteroids for maintenance therapy and budesonide cannot be used for more than 4 months. The group of drugs that are recommended to maintain treatment are biological products such as anti-TNF, but because of the risk of forming antibodies against the drug causing loss of treatment response, the combination with immunomodulatory drugs should be Consideration. In patients using other biological products such as Vedolizumab, Natalizumab, Ustekinumab, if remission is achieved, maintenance therapy can be achieved, but it is important to note that in the case of Natalizumab, periodic monitoring is required to ensure that the patient not infected with JC virus.
5.Risk of postoperative recurrence of Crohn's disease
The main risk factors for postoperative recurrence in Crohn's have been established to include: smoking (particularly in women), simple fistula or abscess-induced fistula, perforation, and patients with a history of surgery. technique at least 2 times before. In addition, there are a number of other factors such as the time from diagnosis to surgery < 10 years, damage to both the ileum and colon with long lesions, and the need for preoperative corticosteroid therapy. Patients who do not smoke, do not have fistulae, and have no previous surgical history are a group of low risk factors for recurrence after surgery. In this group, there is no need for postoperative treatment and periodic follow-up with colonoscopy every 6 months. In non-smokers with no history of surgery or previous medical therapy but with fistula lesions, thiopurine therapy should be followed, followed by colonoscopy every 6 months. If there are lesions on colonoscopy, anti-TNF should be treated.
6.Medications that should be used after surgery
Patients with a history of surgery within 10 years who should be treated with anti-TNF after surgery can consider combining with immunomodulatory drugs and periodically monitoring with colonoscopy every 6 months. Mesalamine is safe but does not provide much benefit in the prevention of recurrence in patients with Crohn's after surgery. A meta-analysis showed that masalamine reduced clinical symptom recurrence and endoscopic severity, but the effect was not significant. However, this can still be considered a reasonable option if the patient cannot use immunosuppressive drugs. Imidazole antibiotics such as metronidazole, ornidazole can be prescribed at a dose of 1-2g/day for patients with Crohn's having small bowel resection. The use of metronidazole has been shown to be effective in preventing recurrence of severe lesions on endoscopic surgery 3 months after surgery and in preventing recurrence of clinical symptoms after 1 year. Ornidazole was also effective in reducing clinical symptom recurrence after 1 year. Some authors suggested using a combination of metronidazole for 3 months with azathioprine for 12 months after surgery and noted an improvement in postoperative endoscopic lesions.

Thiopurine has been shown to be more effective in preventing recurrence of both clinical symptoms and endoscopic lesions than mesalamine or placebo. However, in severe endoscopic recurrent lesions, thiopurine is of little benefit. For high-risk patients, anti-TNE should be started early within 4 weeks of surgery and, although there is insufficient evidence, combination with immunomodulators to induce an immune response and prevent Prevention of antibody formation with drugs recommended by the American Gastroenterology Association.
Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, diseases that cause chronic diarrhea, Crohn's disease... Along with that, at Vinmec Hospital, screening for gastric cancer and gastric polyps is done through gastroscopy with Olympus CV 190 endoscope, with NBI (Narrow Banding Imaging) function for The imaging results of mucosal pathology analysis are clearer than conventional endoscopy, detecting ulcerative colitis lesions, early gastrointestinal cancer lesions... Vinmec Hospital with facilities Quality and modern equipment and a team of experienced experts, always dedicated to medical examination and treatment, customers can rest assured with gastroscopy and esophagogastroduodenoscopy at Vinmec International General Hospital. .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.