This is an automatically translated article.
Diabetic retinopathy is a condition characterized by damage that occurs in the retina. This is a complication caused by diabetes (diabetes mellitus) and the consequences can lead to impaired vision, even blindness.
1. What is diabetic retinopathy?
Diabetes or diabetes is a disease associated with a chronic disorder of glucose metabolism. This is one of the three fastest growing non-communicable diseases (including cancer, cardiovascular disease, and diabetes). Diabetes causes many complications in the eyes, heart, kidneys, nerves. In which, eye complications are common with a high rate.
The retina is the nerve fiber layer of the eye, which plays a role in receiving light, the images the eye receives to the brain and vice versa, has the effect of transmitting images that the brain can analyze to the eye, in which the macula is the most important for the clearest picture.
Diabetic retinopathy caused by diabetes. It occurs most often in cases of diabetes that progress over a long period of 10 to 15 years.
Diabetic retinopathy is the most common cause of blindness between the ages of 20 and 65.
The risk of diabetic retinopathy depends on various factors such as duration of diabetes, blood glucose level and other factors (eg, high blood pressure, hyperlipidemia, kidney disease, pregnancy, intraocular surgery) that may increase the risk and severity of diabetic retinopathy .
Bệnh võng mạc tiểu đường do bệnh lý tiểu đường gây ra
2. Diabetic retinopathy classification
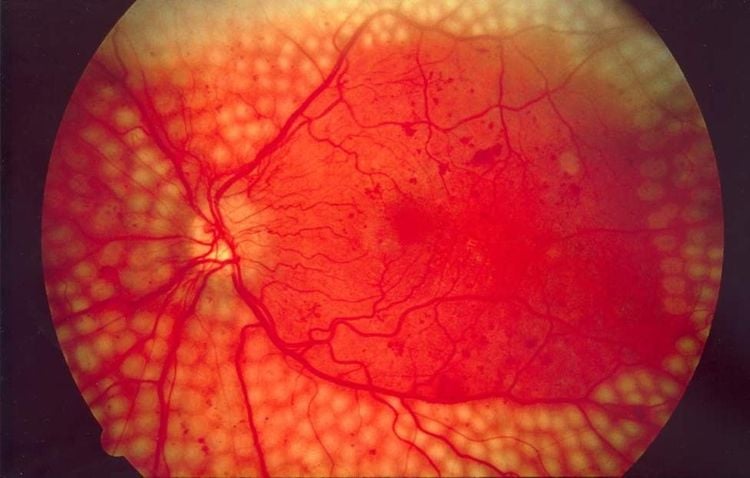
2.1. Onset retinopathy is an early stage of diabetic retinopathy that progresses slowly over a long period of time. At this stage, small hemorrhagic spots with fatty deposits will appear in the retinal area.
Most people with diabetic retinopathy will not lose their vision, but will gradually decline without realizing it. In some cases, blood vessels leak in the macula, which is the central part of the retina that provides central vision and causes vision loss.
2.2. Proliferative retinopathy Proliferative retinopathy develops from primary retinopathy. This is the cause of most cases of vision loss in people with diabetes. New blood vessels will form on the surface of the retina and optic nerve. These blood vessels are fragile and bleed into the vitreous cavity. Scar tissue can also form from broken blood vessels causing the retina to pull away and lead to complete loss of vision. New blood vessels can also form in the iris causing glaucoma (also known as glaucoma) and this condition is a possible cause of blindness.
When bleeding occurs in the stage of proliferative retinopathy, the sufferer feels like seeing through fog, flies or loses vision completely. Although there are no accompanying signs of pain, this is a serious stage of diabetic retinopathy and requires immediate treatment.
3. Treating Diabetic Retinopathy
Depending on the stage of diabetic retinopathy, there will be appropriate treatment methods such as: monitoring, laser photocoagulation of the retina, intraocular injection of angiogenesis inhibitors (anti-VEGF) or corticosteroids. against macular edema, surgical intervention.
3.1. Diabetic retinopathy treatment process Measure vision for people with the disease. General eye examination includes: Tonometry, eyelid examination, corneal conjunctiva, anterior chamber, iris, vitreous to have a general assessment of eye function. Apply a pupil dilator to examine the vitreous and retina of the eye. Fundus color imaging to identify eye lesions in the early stages. If fundus imaging has appeared lesions, then proceed with fluorescein angiography. Its role is to detect microaneurysms, hemorrhages, exudates, ischemia, and neovascularization very accurately. In addition, you may be ordered by the treating doctor to have an OCT scan. This is an extremely modern method to evaluate macular edema and damage of the central retina. Fluorescein angiography and OCT are also used to monitor the progression of diabetic retinopathy. 3.2. Laser treatment of retinal photocoagulation The effectiveness of laser methods in the treatment of diabetic retinopathy is:
Directly destroy the ischemic retina where the proliferative factors of blood vessels are produced. The laser destroys radiopaque cells and oxygen-consuming retinal pigment epithelial cells. The effect improves the oxidation of the inner retinal layer and reduces the stimulation of the production of neovascular proliferative factors. Release of angiogenesis inhibitory factor normally located in the pigment epithelium. Depending on the damage of the retina, laser photocoagulation techniques can be selected as follows: Focal laser, grid laser, and panretinal laser. The extent of total retinal photocoagulation depends on the progression of proliferative diabetic retinopathy.
After the laser is done, you may have a feeling of glare, decreased vision, and signs of flashing. However, these symptoms are only temporary and will go away quickly. After laser treatment, you need to be periodically re-examined, checked for the first time after 4 to 8 weeks and then, depending on the extent of the damage, the doctors will re-examine and follow up closely.

Chụp mạch huỳnh quang và OCT còn để theo dõi diễn tiến của bệnh võng mạc tiểu đường
3.3. Intraocular injections Intraocular drugs in the treatment of diabetic retinopathy, including corticosteroids or anti-VEGF (Lucentis, Avastin, Pegabtanib) have the effect of preventing neovascularization and macular edema.
3.4. Vitrectomy Working in the optical environment: The leading causes of vitreous hemorrhage due to diabetes are heavy bleeding that does not dissolve, bleeding with vascular proliferation. Exclude retinal vitreous tugging, pulling caused by proliferation of vitreous retina, fibrovascular membrane. Treatment of other concomitant pathological processes such as cystic macular edema, retractile retinal detachment and vitreous proliferative membrane.
4. Prevention of diabetic retinopathy complications
People with diabetes can prolong disease-free time or slow the progression of diabetic retinopathy by maintaining stable blood sugar and blood pressure levels. There are 2 indicators that people being treated for diabetes need to pay attention to: blood sugar and HbA1c. Besides, the blood lipid index, blood pressure, ... also need to be monitored.
As recommended by medical experts, you should keep your blood sugar at a safe level of less than 7.0 mM/L with an HbA1c < 6.5%.
In addition to controlling blood sugar, you also need to pay attention to eye nutrition and reasonable living. You should add foods rich in antioxidants (vitamins E and C, beta-carotene, ...) or substances that increase microvascular circulation. At the same time, different types of diabetes can experience retinal complications, so when you have the disease, you should have regular eye exams every 3, 6 or 12 months to detect damage to the retina early. .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.