This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Huynh Kim Long - Emergency Resuscitation Doctor - Emergency Resuscitation Department - Vinmec Da Nang International General Hospital. Dr. Huynh Kim Long has extensive experience in the treatment of Resuscitation - Emergency and Acute Stroke in adults.Acute renal failure is defined as a sudden decrease in glomerular filtration rate. This is a common problem in resuscitation with an incidence varying from 20% to 70%. The clinical manifestations of acute renal failure in resuscitation vary widely from case to case according to the site of renal injury. However, the sudden decrease in kidney function will disturb the intracellular environment as well as endanger life if not corrected in time.
1. Overview of treatment of acute renal failure in resuscitation
The best treatment for acute renal failure in resuscitation is to find the cause, recognize the risk factors early, and actively prevent existing ones. Specifically, factors that reduce the perfusion time to the kidney causing acute renal failure will be recognized quickly when there is a lack of cardiac output. Therefore, the therapeutic goal of maintaining an adequate endovascular effective volume and avoiding nephrotoxicity is the key to preventing true acute renal failure.In general, there is no one-size-fits-all management strategy for all patients with acute renal failure. The components of acute renal failure in basic resuscitation include maintaining intravascular volume, optimizing cardiac function, releasing mechanical obstruction if present, and discontinuing stimulant drugs that cause acute interstitial nephritis. .
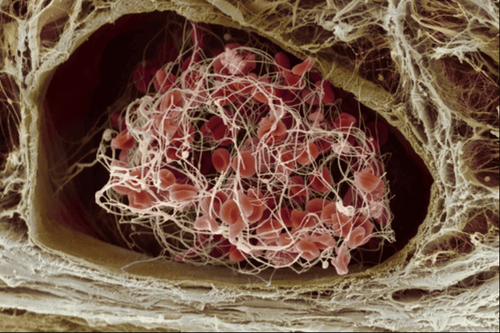
In the case of optimized cardiac output and volume status, if the patient remains oliguria, the physician may prescribe additional diuretics to improve urine output. In addition, additional use of renal vasodilators, including dopamine and fenoldopam, should also be considered to help increase renal blood flow. However, these measures are no longer recommended, because there is no evidence to improve glomerular filtration rate or in-hospital mortality in patients requiring intensive care.
The components of acute renal failure in resuscitation are detailed below.
2. Ensure effective circulating volume
In the resuscitation setting, fluid balance is considered the fifth survival parameter. If clinical assessment suggests an intravascular volume deficit, the first thing to do is to optimize hemodynamic status and to adjust the effective intravascular volume for renal function. Thereby, the reduction of kidney damage will be actively controlled.The ways to add fluids to the resuscitated patient are usually through fluids and are done while monitoring urine output, blood pressure, or changes in central venous pressure to avoid excessive perfusion. In contrast, for patients with reduced intravascular volume due to increased vascular permeability, fluid escapes from the interstitium, colloid solutions such as albumin should be used to maintain osmotic pressure as well as circulating volume. effective. In addition, albumin infusion is also indicated in patients with cirrhosis associated with acute renal failure in hepatorenal syndrome and early combination with vasopressors is considered.

3. Consider taking vasopressors when indicated
If fluid resuscitation is adequate, or if the patient has contraindications to fluid resuscitation, such as heart failure, or if the patient has an increased vascular permeability that causes fluid to leak into the interstitium, as in septic shock, treat Acute renal failure in the ICU now requires vasopressors. In particular, norepinephrine is the vasopressor of choice with the ability to rapidly improve mean arterial pressure and the target should be in the range of 65 to 70 mmHg.However, in patients with chronic hypertension, the target mean arterial pressure may be higher than 80 to 85 mmHg and the dose of vasopressor should be carefully adjusted as soon as the target is reached. OK, reduce the dose as soon as possible. Furthermore, in patients with hepatorenal syndrome, all vasopressors should be used only in combination with albumin therapy.
4. Combined with diuretics
Previous studies have demonstrated the ability to improve glomerular filtration rate with the use of diuretics in acute renal failure. Although diuretics may cause an initial increase in serum creatinine, their role is to rapidly restore urine volume, indirectly correcting disturbances of endothelial metabolism and electrolyte balance.How to use diuretics to start will depend on the patient's condition. Usually the route of administration chosen is a continuous intravenous infusion with a titration of the drug concentration gradually increasing from 1.0; 1.5 mg of furosemide and increased per kg of body weight during the oliguria phase. Then, when the urine output has recovered, the diuretic is gradually reduced, converted to the intravenous route. However, during the use of diuretics, it is necessary to closely monitor the water-export balance because the diuretics themselves will increase the functional burden, delaying recovery in acute renal failure. Despite this, in patients with acute renal failure in a cardiovascular syndrome with decompensated heart failure, early use of loop diuretics may be considered as a means of preventing progression to renal failure if heart failure persists. unfavorable progress.

5. Avoid delaying renal replacement therapy
Historically, the decision to initiate renal replacement therapy for acute renal failure in resuscitation has often been based on clinical features of the patient such as volume overload and serum biochemical abnormalities. such as uremia, hyperkalemia, metabolic acidosis if the above medical management measures are not effective.However, this holistic approach should be based on the patient's clinical context and be individualized. When the patient's condition is critical, acute renal failure is the consequence in this situation and it is difficult to wait for the time when the medical measures are effective, the indication for dialysis at this time is to avoid delay. The emergency dialysis intervention not only helps to limit further damage to kidney cells, but also quickly adjusts the homeostasis as well as reduces the burden on cardiovascular or cardiopulmonary function if continuous dialysis is combined with weekly dialysis. outside the body.
In summary, acute renal failure in resuscitation is a predisposing factor to poor prognosis for patients. In critically ill patients, acute renal failure is the result of a variety of causes; Therefore, the best treatment is always proactive prevention. However, the optimization of hemodynamics, the combination of diuretics, vasopressors, as well as timely renal replacement will also contribute to improved renal function for patients in intensive care.

Health checkup package diamond general health check-up package Vip special health check-up package Comprehensive general health check-up package Standard general health check-up package Patient's examination results will be returned to your home. After receiving the results of the general health examination, if you detect diseases that require intensive examination and treatment, you can use services from other specialties at the Hospital with quality treatment and services. outstanding customer service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.