This is an automatically translated article.
Smoking is not only a cause of lung cancer, but it also causes many other lung diseases such as chronic obstructive pulmonary disease, asthma...Effects of Medicines on Lung Function When we breathe in, air enters the upper respiratory tract through the nose and mouth, where the air is filtered, heated, and warmed. Inhaled air passes through the trachea into the lungs.
In each lung there is a bronchial system, the main bronchus is like the main branch of a tree with small branches being the bronchi, after 17 - 20 times dividing into terminal bronchioles, from the bronchioles That leads to little sacs of gas called alveoli, which are like bunches of grapes. In the alveoli, gas exchange takes place. The blood will exchange CO2 for O2 to the body's organs.
The respiratory system has several protective barriers against diseases. The filtration process in the upper respiratory tract helps prevent bacteria, viruses and irritants from entering the lungs from the outside. The trachea and lung tissue produce mucus to help pick up and carry dirt out. The mixture of mucus and impurities is carried out by tiny hairs called cilia, which move very rapidly upwards, in some areas the speed of the feathers is as high as 1,000 times per day. one minute.
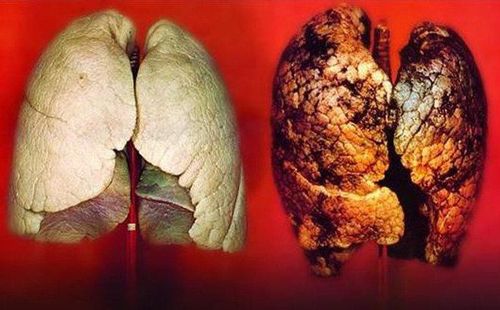
Thuốc lá gây ra nhiều bệnh ảnh hưởng tới sức khỏe con người (Ảnh minh họa)
When smoke enters through the mouth, the smoker inadvertently bypasses the first defense mechanism that is the filtering process in the nose. Smokers often excrete more sputum than non-smokers, but the ability to remove sputum out of the respiratory tract is less. This is because the ciliary system in paralyzed smokers is even destroyed. Smoking also alters the structure of the mucous glands and thus the composition of the mucus. Sometimes the mucous glands become blocked, reducing the ability to excrete sputum. As a result, the mucus in smokers is contaminated with toxic substances and is trapped in the lung tissue, hindering the circulation of gas exchange.
The lungs of smokers have reduced surface area and reduced capillaries, which means that blood flow through the lungs is reduced. This leads to a decrease in the supply of nutrients and oxygen needed by both the lung parenchyma and other organs in the body to maintain their health and normal function.
Smoking also causes a phenomenon called airway hyperresponsiveness, due to the effects of toxic substances in smoke, airway constriction. When this happens, both inhalation and exhalation are obstructed in the smoker and thus crackles, crackles and possibly difficulty breathing are formed.
In smokers there are many variable functional parameters of ventilation, in which first second forced expiratory volume (FEV1) is greatly reduced.
Secondhand smoke reduces lung growth and causes inflammation of the lung tissues in children and adolescents as demonstrated by a slower rate of increase in FEV1. At the age of 20 - 30 when smoking, lung damage is different. When at this stage of life the lung grows to a plateau. In smokers this developmental period is shortened and causes smoking-related diseases to appear early. At the age of 30, if smokers, the rate of decrease in FEV1 will double (about 40ml/year) compared to non-smokers (about 20ml/year). Younger smokers had a shorter time smoking to cause respiratory illness than those who started smoking at a later age.
Chronic Obstructive Pulmonary Disease Chronic Obstructive Pulmonary Disease (COPD) is the term used to describe lung lesions associated with airway obstruction. Chronic Obstructive Pulmonary Disease (COPD) is characterized by irreversible obstructive airways disease, confirmed by spirometry with incompletely reversible bronchodilator testing.
According to WHO, in the world in 2001 there were about 600 million people with COPD. The disease progresses over many years and eventually leads to congestive heart failure and death. COPD is the 4th leading cause of death worldwide. The association between COPD and smoking is as strong as with lung cancer.
Tobacco is the most important cause of COPD, about 15% of smokers will have clinical symptoms of COPD and 80-90% of people with COPD are smokers. Smoking makes other risk factors for this disease stronger. In particular, smokers are worse affected by environmental pollution, infections and exposure to toxic fumes than non-smokers. Smokers are 10 times more likely to die from chronic obstructive pulmonary disease than non-smokers.
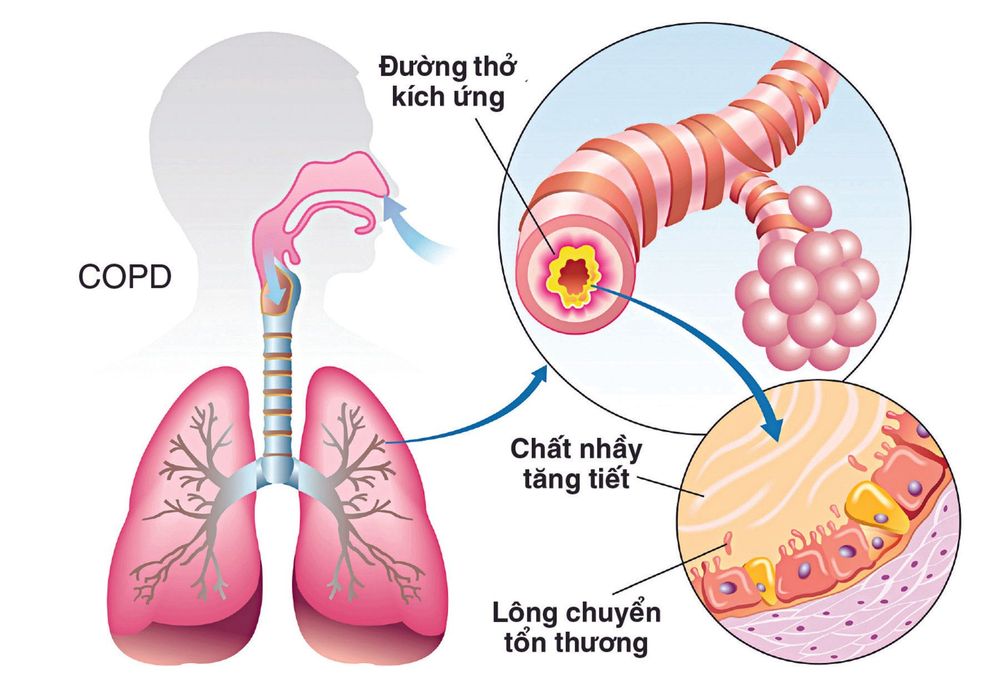
Người hút thuốc có tỉ lệ tử vong do bệnh phổi tắc nghẽn mạn tính cao gấp 10 lần so với người không hút thuốc.
Smoking is not the cause of an asthma attack, but it does make asthma worse. People with asthma who smoke will have increased sputum production, decreased bronchial ciliary movement, increased susceptibility to infections, increased release of fast-acting allergens, and destruction of small airways. The mortality rate among current or former smokers with asthma is more than twice that of non-smokers.
Respiratory tract infections Smokers are more prone to respiratory infections than non-smokers, and they often get worse. Children whose parents smoke are more likely to have respiratory illnesses than children whose parents don't smoke.
Smokers not only get pneumonia more often, they also die more often.
Pregnant women with pneumonia who smoke more than 10 cigarettes a day have a worse prognosis than those who do not smoke (mortality of mother, child...).
Smokers also get the flu. The flu vaccine is less effective in smokers, and the death rate from the flu is much higher in smokers than in non-smokers.
According to Dr. Ho Xuan Cung - Life Health