This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Inflammatory bowel disease (IBD) represents a group of chronic inflammatory disorders involving the colon, small intestine (SB) and the entire gastrointestinal tract and includes Crohn's disease (Crohn's disease), ulcerative colitis (Crohn's disease), and ulcerative colitis (Crohn's disease). UC) and unclassified entities.
Abbreviations:
Inflammatory bowel disease (IBD) Crohn's disease (Crohn's disease) Small bowel (SB) Capsule endoscopy (CE) DAE: assistive small bowel endoscopy; DBE: Dual Balloon Boweloscopy; SBE: Single-balloon endoscopy;
1. Overview of inflammatory bowel disease
Crohn's disease is an immune-mediated chronic inflammatory disease that usually involves the ileum and the ileum, but at the time of diagnosis it may be confined to the small intestine, as seen in about 30% of patients with Crohn's disease. , especially young patients. Small bowel Crohn's disease alone can be difficult to diagnose and manage for a number of reasons:
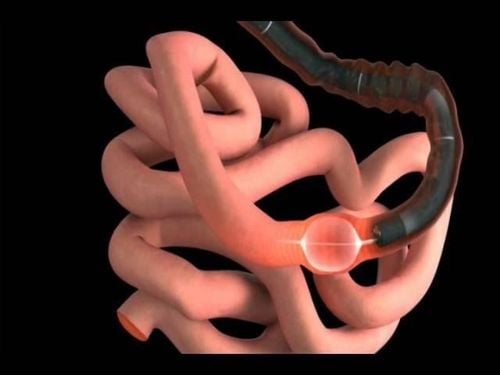
First, small bowel Crohn's disease alone is more difficult to reach with endoscopy, making it easier to miss a diagnosis of small bowel Crohn's disease alone with routine endoscopy, which contributes to the delay in diagnosis as observed in many patients with Crohn's disease.
Second, small bowel ulcers caused by infections (such as tuberculosis) or medications can sometimes be difficult to distinguish from Crohn's disease.
Third, compared with other phenotypes, small bowel Crohn's disease alone is associated with an increased risk of recurrence and serious development.
Fourth, small bowel cancer associated with small bowel Crohn's disease is a rare but difficult problem because only a small number of these cases are diagnosed preoperatively and at an early stage.
Finally, in the pediatric population, small bowel Crohn's disease alone is of particular clinical relevance because of its negative impact on pubertal growth and development. Therefore, objective evaluation of the small intestinal mucosa is essential in distinguishing Crohn's disease from other bowel diseases for decision making and planning for follow-up.
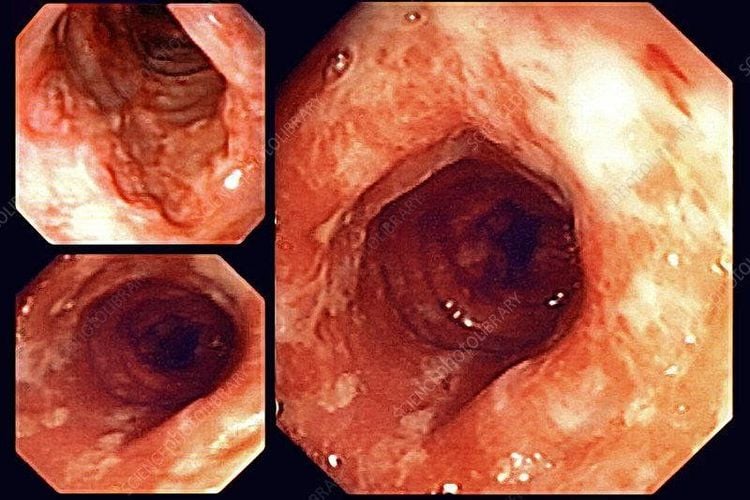
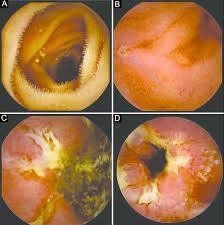
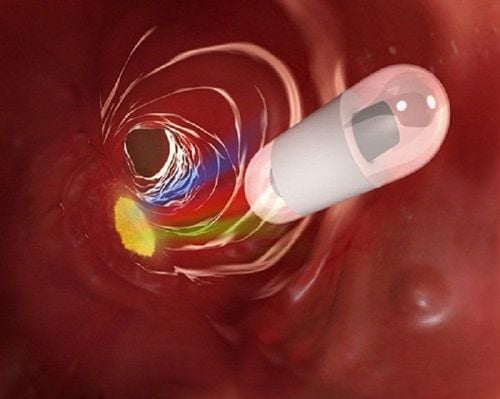
2. Small bowel endoscopy in adult patients with known inflammatory bowel disease complicated by gastrointestinal narrowing
Four studies evaluated the impact of Balloon Assisted Small Boweloscopy in adults with known and complicated IBD. Mensink et al evaluated the clinical impact of endoscopic small bowel assessment in patients with known Crohn's disease and clinically suspected small bowel functioning. They retrospectively analyzed 52 single-balloon endoscopic procedures performed in 40 adult patients. 24 patients (60%) presented with active enteritis on a macroscopic basis, and 18 of them (75%) required conversion to therapy with persistent clinical improvement in 83% of patients after time. Median follow-up was 13 months. In particular, of the 18 patients, 11 received anti-TNF therapy, 2 switched from infliximab to adalimumab, 1 received steroid therapy, 2 had bowel resection, and 2 underwent dilation. ball to solve the narrow spot.
In the study from Navaneethan et al., Balloon-Assisted Enteroscopy System was performed in 43 adult patients with a definitive diagnosis of Crohn's disease whose primary hallmark was assessment of disease activity and severity. in unresolved Crohn's disease, anemia, or unclear gastrointestinal bleeding, confirm and treat small bowel severity diagnosed on radiographic examination, and assess the activity and extent of Crohn's disease in patients after surgery. Balloon-assisted endoscopic system had an impact on the clinical management of 23 patients (53.4%): 18 patients (41.8%) had active inflammation with ulceration or ulcerative scarring. stenosis leading to conversion to medical or surgical therapy, 5 (11.6%) with stenosis noted in the absence of active ulcers that underwent EBS endoscopic balloon dilation for management treatment of obstructive symptoms. Overall, 13 patients (30%) required surgery: Two were due to lack of other treatment strategies, five were due to medical treatment failure, five were of patient choice , and one from bowel perforation after balloon-assisted colonoscopy. Finally, the authors found that the rate of agreement between CT or MRI of the bowel and findings with a balloon-assisted endoscopic system was higher (75.6%) in patients with diagnosed Crohn's disease.
3. Efficacy of small bowel endoscopy in the management and treatment of inflammatory bowel disease
In the study by Rahman et al., the authors analyzed the diagnostic results and clinical impact of dual-balloon colooscopy on the management of 38 adult patients with known Crohn's disease and clinical suspicion of small bowel disease activity. In this setting, the diagnostic yield was 87% (33/38 patients), indicating active disease in 11 patients (29%), 5 patients with obstructive Crohn's disease (13%), 3 ( 8%) had functional obstruction due to fixed/spasmodic bowel, 3 (8%) had anastomosis ulcer, and 2 (5%) had a nonspecific ulcer. Double-balloon endoscopic examination of small bowel was normal in 9 cases (23.6%). Thus, dual-balloon enteroscopy resulted in a change in the clinical direction of treatment for 82% of patients with known Crohn's disease. Thirteen patients (34%) required an increase in drug dose or switch therapy or surgery, and three patients (8%) underwent endoscopic balloon stenosis without any associated complications.
4. The role of small bowel endoscopy in the assessment of complications of inflammatory bowel disease
Holleran et al evaluated the diagnostic and clinical outcomes of the use of single-balloon enteroscopy in 39 patients with small bowel Crohn's disease performed. In this setting, the diagnostic yield was significantly higher than in adult patients with suspected Crohn's disease (77% vs 39%, P < 0.01). The most frequent findings were ileostomy or anastomosis in 38% and 26%, and active ileitis in 21% of patients. SBE had an immediate clinical impact in 69% (n = 33) of patients, including spasmodic relaxation in 27%, medication adjustment in 48%, and referral for surgical resection in 6%. Long-term follow-up (median duration 11 months, range 3-22 months), performed in 34 patients (65%) out of 52 patients, showed significant variation in Harvey- Bradshaw mean 6.6 to 4.2 after procedure (P < 0.0001).
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:Fong SC, Irving PM. Distinct management issues with Crohn's disease of the small intestine. Curr Opin Gastroenterol. 2015;31:92-97. [PubMed] [DOI] Sauer CG, Kugathasan S. Pediatric inflammatory bowel disease: highlighting pediatric differences in IBD. Med Clin North Am. 2010;94:35-52. [PubMed] [DOI]3. Hall B, Holleran G, McNamara D. Small bowel Crohn's disease: an emerging disease phenotype? Dig Dis. 2015;33:42-51. [PubMed] [DOI]4. Peyrin-Biroulet L, Loftus EV Jr, Colombel JF, Sandborn WJ. The natural history of adult Crohn's disease in population-based cohorts. AmJ Gastroenterol. 2010;105:289-297. [PubMed] [DOI]5. Pimentel M, Chang M, Chow EJ, Tabibzadeh S, Kirit-Kiriak V, Targan SR, Lin HC. Identification of a prodromal period in Crohn's disease but not ulcerative colitis. AmJ Gastroenterol. 2000;95:3458-3462. [PubMed] [DOI]6. Giovanni Di Nardo, Gianluca Esposito et al., Enteroscopy in children and adults with inflammatory bowel disease, World J Gastroenterol. Oct 21, 2020; 26(39): 5944-5958