This is an automatically translated article.
The article is written by Master, Doctor Mai Vien Phuong - Head of Department of Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalMesenteric embolism is a disease without typical and specific symptoms, caused by the blockage of blood vessels supplying the small and large intestines. Emergency treatment and treatment play an extremely important role in helping patients reduce the risk of death.
1. The role of exploratory laparotomy in the diagnosis of mesenteric embolism
Mesenteric embolism is a disease that often has no specific clinical signs and symptoms, so most patients are often diagnosed at a too late stage, when the intestines have been infarcted. In addition, the disease often occurs in elderly patients and is accompanied by complicated medical conditions that affect the current treatment, which is mainly surgical re-establishment of blood flow and excision of the blood vessels. intestines cannot survive. During surgery, two factors need to be determined: the extent of the intestinal lesion and the circulation of the superior mesenteric artery.
The extent of the intestinal lesion is partly related to the cause of the mesenteric embolism. When thrombus overlaps with chronic atherosclerotic plaque at the base of the superior mesenteric artery, it usually results in damage to the entire small intestine and the right colon, the portion of intestine that is fed by this artery. When there is embolism in the main body of the superior mesenteric artery, there is usually an uninjured proximal small bowel, and in distal embolism, in the branches of the superior mesenteric artery, only ischemic lesions in the mesenteric artery occur. bowel sections are affected.
Exploratory laparotomy, to establish the diagnosis and assess the extent of intestinal ischemia, remains the gold standard. The intestines often turn purple or burgundy-black spreading. It is rare to find a perfectly normal bowel, but if this is the case, it is important to confirm the presence or absence of a pulse in the main body of the superior mesenteric artery at the base of the mesentery or its branches. Bowel performance is dependent on the degree of collateral circulation and the duration of ischemia. In contrast, cases of venous thrombosis are characterized by limited portions of the bowel and adjacent mesentery with edema, fluid retention, and discoloration, but with palpable superior mesenteric artery and its branches. its.
2. Laparoscopy
With the advent of laparoscopic surgery, in addition to being used to treat most diseases of the abdominal organs, it is also safely and effectively applied in the diagnosis of acute abdominal conditions. Surgery is difficult to confirm the diagnosis. However, the disadvantage of this method is that it is difficult to perform when the patient arrives in the late stage, when the bowel is completely distended and the pulse of the artery cannot be palpable during surgery.
3. Treatment of mesenteric embolism
Exploratory laparotomy without any management may be considered in cases of extensive intestinal infarction due to mesenteric embolism in which cases, if bowel resection is performed, the patient will also die postoperatively, followed by only provisional treatment. Surgical treatment of mesenteric embolism is aimed at two purposes, firstly, to restore intestinal blood flow. the second, is to remove the parts of the intestine that are not viable. This order must be ensured, because parts of the intestine with doubt of viability can be restored after the blood vessels are circulated. The method of revascularization is usually thrombectomy or bridging.
4. Methods and techniques of mesenteric vascular surgery
Obstruction of superior mesenteric artery due to embolism. After midline laparotomy, exposure of the superior mesenteric artery in the small bowel mesentery is the standard technique for performing thrombectomy. The transverse colon and the greater omentum were brought forward and made a transperitoneal incision at the base of the transverse colon and followed proximally to its origin at the superior mesenteric artery. The superior mesenteric artery was dissected just below the lower border of the pancreas, the transverse mesentery. Perform thrombectomy with a balloon, Fogarty catheter, through a proximal transarterial incision.

5. Obstruction of superior mesenteric artery due to thrombosis
During laparotomy, it can be difficult to distinguish between embolism and thrombosis, which the surgeon needs to decide whether to perform catheter or balloon thrombectomy as described above. However, this technique is not recommended in cases of thromboembolism, because of the risk of rapid re-occlusion. In the emergency setting, the authors recommend re-implantation of the inferior pancreatic mesenteric artery with a terminal-lateral renal inferior abdominal aorta or performing a bypass of the abdominal aorta, mesenteric artery, or iliac artery rather than Attempts to perform thrombectomy of the narrow proximal aorta with difficulty. Usually an artificial graft is used, but in cases of bowel necrosis or perforation requiring bowel resection, the recommended graft is the patient's great saphenous vein.

6. Diagram of superior mesenteric artery–abdominal aorta
In patients with chronic mesenteric ischemia, stenting or endovascular resection (endovascular intervention) is technically feasible with low complication rates, but experience is very limited in these conditions. emergency situations. Batelier et al retrospectively reviewed 82 patients with acute mesenteric ischemia due to mesenteric artery embolism, 34 patients requiring only thrombectomy, 20 patients requiring thrombectomy and bowel resection. Patients with thrombectomy alone had a perioperative mortality rate of 35%, and patients with thrombectomy and ileostomy had a perioperative mortality rate of 68%. The authors concluded that early diagnosis and surgical removal of the thrombus are considered to have better outcomes, because the need for bowel resection is avoided. To avoid complications of late bowel necrosis, after exploratory laparotomy and mesenteric vascular reconstruction, it is necessary to accurately assess the viability of the intestine during surgery by color assessment. of the intestine, observing bowel movements, palpating the mesenteric vessels and bleeding from the cross-section. This is considered the best way to assess the bowel with a sensitivity of 91% and a specificity of 82%. However, it is a subjective measure and depends on the assessor.
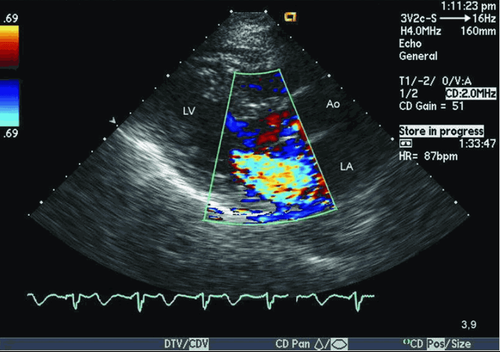
Other methods have also been applied to assess intestinal viability during surgery with color Doppler ultrasound or intravenous fluorescein and visualization of the intestine under Wood's lamp.
Another commonly used approach is second look laparotomy, which is planned during the first surgery, and is done within 24-36 hours after surgery. in most cases to assess the viability of the remaining intestine and anastomosis. If there are signs of continued bowel necrosis, further resection is performed.
Although, some authors argue that this is not necessary in all cases. The decision to anastomose immediately or remove both ends of the intestine after resection of the necrotic bowel is based on the general condition of the patient and the health of the remaining bowel. In general, if the patient is clinically stable, and the small bowel is well perfused, anastomosis should be done immediately.
Mortality is related to the extent of the bowel infarct. Thrombotic obstruction is more likely to occur proximal to the superior mesenteric artery than embolic obstruction and is more often associated with a more extensive intestinal infarction. There is a lack of studies on the determinants of widespread intestinal infarction, except for the anatomical location of the obstruction. The reported mortality rate of acute superior mesenteric artery occlusion is highly variable, reflecting the heterogeneity of the study samples. Patients with arterial thromboembolism appear to have a worse prognosis than patients with thromboembolic occlusion. Klempnauer et al. reported that the treatment outcome of acute mesenteric ischemia due to occlusion of the mesenteric artery or vein resulted in 66% postoperative mortality and 50% of surviving cases. mortality after 5 years and 20% of cases with short bowel syndrome without parenteral nutrition.
Vinmec International General Hospital is a high-quality medical facility in Vietnam with a team of highly qualified medical professionals, well-trained, domestic and foreign, and experienced. A system of modern and advanced medical equipment, possessing many of the best machines in the world, helps to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of effective doctors. most fruitful.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
REFERENCES
Nguyen Tuan* , Nguyen Tan Cuong. Diagnosis and treatment of mesenteric artery occlusion. Medicine Ho Chi Minh City. 2008 - Volume 12 - Issue 3 Acosta S, Ugren M, Sternby N-H, et al (2004), “Incidence of acute thrombo-embolic occlusion of the superior mesenteric artery. A population-based study”, Eur J Vasc Endovasc Surg, 27, pp.145-150. Acosta S, Ugren M, Sternby N-H, et al (2005), “Mesenteric venous thrombosis with transmural intestinal infarction: A population-based study”, J Vasc Surg, 41, pp.59-63. Acosta S, Ugren M, Sternby N-H, et al (2005), “Clinical implications for the management of acute thromboembolic occlusion of the superior mesenteric artery. Autopsy findings in 213 patients”, Ann Surg, 241, pp.516-522.