This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Patients often question the role of diet in inflammatory bowel disease (IBD). Despite the interest in this topic, there is little consensus on how to address diet in IBD patients.
Animal studies and population-based human studies serve as the knowledge base for IBD risk associations. Such studies have demonstrated the positive effects of omega-3 fatty acids, amino acids, plant polysaccharides, vitamin D, fiber, fruits, vegetables and fish....
1. Doctor's and patient's wishes in the treatment of inflammatory bowel disease
In a recently proposed IBD patient needs hierarchy, there is a contradiction between the patient's needs and the physician's focus, especially when it comes to the role of diet . Clinicians tend to focus on identifying and achieving treatment goals while patients are often concerned with what they can eat and whether diets are helpful or harmful to their health. with IBD.
Although the role of diet in IBD is increasingly discussed, if at all, consensus on the topic is still limited. In this article, we aim to review several aspects of the function of diet in IBD including its role in changing the epidemiology, pathogenesis, and risk of IBD. We will also look at some of the diets that have been suggested and studied as potential therapies for IBD.
2. Diet in the pathogenesis, risk and outcome of IBD
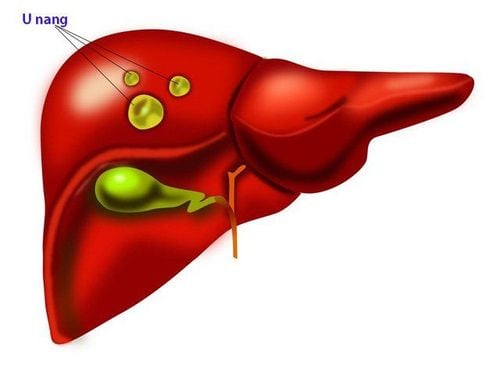
The interplay between diet and IBD has largely been studied through animal models of enteritis and epidemiological studies of IBD risk associations. Animal models have been used to study the pathogenicity of specific dietary components in inducing enteritis. In addition, several large, population-based groups have been used to investigate associations between IBD risk and specific dietary components. Given the limited amount of clinical trial data in the field of dietetics and IBD, these studies provide an important framework for better understanding the interplay between diet and IBD.
2.1 Results of Animal Studies Animal studies investigating high-fat diets in general have demonstrated anti-inflammatory effects. A study in a mouse model of Crohn's ileitis showed that a high-fat diet led to the accelerated development of Crohn's disease due to increased intestinal permeability and altered photoluminescence processes. Furthermore, in a mouse model of sodium dextran sulfate (DSS)-induced colitis, a Westernized high-fat diet resulted in rapid weight loss, an effect magnified by heme supplementation. , an abundant component of red meat. While these studies show anti-inflammatory effects from a high-fat diet, omega-3 fatty acids often demonstrate anti-inflammatory effects.
2.2 Role of the elimination diet (EEN) in the treatment of ulcerative colitis Studies on the elimination diet for the treatment of ulcerative colitis are lacking. A small clinical trial randomized patients with moderate to severe UC to receive total enteral nutrition or total parenteral nutrition (TPN) as nutritional support in addition to medical therapy. This study showed no significant difference in read rate and resection rate between the 2 groups. However, patients who received enteral feeding had fewer frequent and milder adverse events (9% vs 35%, p = 0.046) and fewer postoperative infections (p = 0.028).
2.3 Diets and dietary interventions Other identified diets that have been suggested to have a potential therapeutic role in the treatment of inflammatory bowel disease include diet specific carbohydrate (SCD), gluten-free diet, anti-inflammatory and low-fermentable oligosaccharide, disaccharide, monosaccharide and polyol diet (FODMAP). It should be noted that most of these diets have not been evaluated in a randomized trial, and only anecdotal benefits have been reported.
Role of Specific Carbohydrate Diets Specific carbohydrate diets include only monosaccharides found in fruits and vegetables and exclude disaccharides and polysaccharides found in simple sugars and wheat products. It restricts carbohydrates and processed foods, potentially making it difficult to maintain compliance in the long run.
The carbohydrate diet was originally used to treat celiac disease and suggested that undigested complex carbohydrates make their way into the colon and eventually lead to intestinal damage due to overproduction of bacteria and yeasts. and mucus.
A recent online survey of 417 respondents (47% with CD, 43% with UC, 10% with colitis indeterminate) showed clinical improvement with a carbohydrate diet . Before initiating SCD, 4% of patients reported clinical remission compared with 33% at 2 months and 42% at 6 and 12 months. Abdominal pain occurs in 80% of patients before the onset of SCD, and this incidence decreases to less than 10% at 12 months. Another study by Cohen used capsule endoscopy to prospectively evaluate both clinical and mucosal responses to SCD. Nine pediatric patients with Crohn's disease completed the trial after 10 were enrolled. There were significant improvements in the Harvey-Bradshaw Index (p = 0.007), PCDAI (p = 0.011) and Lewis score (p = 0.012).
Gluten-free diet Similar to the carbohydrate diet, there is a limited investigation of the gluten-free diet in IBD patients, but gluten sensitivity may be common in IBD patients. One study A single-center unit on 102 IBD patients (55 CD, 46 UC) reported gluten sensitivity in 23.6% and 27.3% of CD and UC patients, respectively. A recent cross-sectional study investigated the gluten-free diet using gluten-free dietary questionnaires in 1647 IBD patients participating in a longitudinal internet-based cohort. Results showed that of the 314 (19.1%) participants who tried the gluten-free diet, 65.6% reported improvement in symptoms and 38.3% reported little or no severity. The Anti-Inflammatory Diet (IBD-AID) is based on SCD and selectively eliminates refined sugars, gluten, and starches. Clinical studies on this diet are lacking, with the exception of a small case series of 11 patients, all of whom reported symptom relief with decreased bowel movements after 4 weeks.

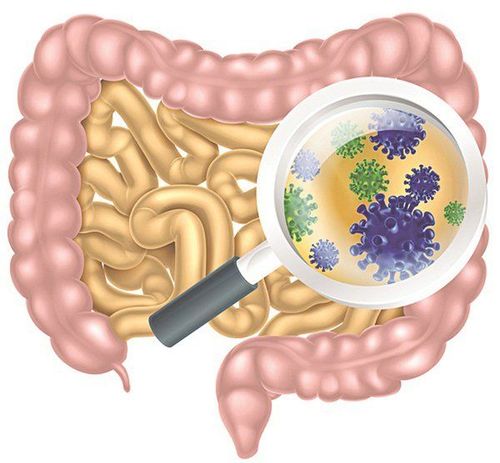
Low-FODMAP Diet The term FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are short-chain carbohydrates that are poorly absorbed from the gastrointestinal tract (GI) in some people and cause gas, bloating, and pain. The low-FODMAP diet was "born" in Australia in 2010 when a team of researchers at Monash University found that limiting foods high in FODMAPs could help relieve common IBS symptoms. stomach, bloating, flatulence, diarrhea and constipation.
The low-FODMAP diet reduces the amount of poorly absorbed carbohydrates that are digested by gut bacteria to produce digestive symptoms. Given the significant impact of functional gastrointestinal symptoms on IBD patients, 68.69 low-FODMAP diets have been considered a dietary intervention in IBD patients, especially in those with symptoms with unstable IBD.
However, several studies have investigated low-FODMAP diets in IBD. A study of 32 patients with unstable IBD and functional gastrointestinal symptoms showed that challenge with fructan, a fermentable carbohydrate, resulted in severe pain, bloating, and urge to pass stools. Another prospective study investigating a low-FODMAP diet in IBD (n = 30), in addition to irritable bowel syndrome and celiac disease, showed an improvement in Rome III endpoints across all subjects, including IBD patients. Another study used a prospective survey to assess clinical response to a low-FODMAP diet and showed symptom improvement in 78% at week 6 with improved stool consistency (p = 0.002) and frequency (p < 0.001) compared to baseline.
3. The role of fish oil in the treatment of inflammatory bowel disease
Finally, it should be noted that older clinical trials have studied fish oil supplementation as a diet-related IBD therapy. An initial, double-blind, placebo-controlled crossover trial of fish oil supplementation with omega-3 fatty acids showed no significant difference in the clinical performance of CD and UC patients.
2 additional randomized controlled trial showing no statistically significant benefit in ulcerative colitis severity based on histopathology score or mucosal cytokine levels and incidence in remission without corticosteroids. However, a randomized controlled trial of an oral supplement enriched with fish oil, soluble fiber, and antioxidants was associated with improved clinical response and reduced need for corticosteroids in 121 UC patients compared with placebo (p < 0.001).

4. Conclusion
As we learn more about the role of diet in IBD, signals from the existing literature demonstrate the positive and harmful effects of a number of different dietary factors. Animal studies and human studies of risk associations suggest a possible protective role for omega-3 fatty acids, amino acids, plant polysaccharides, vitamin D, dietary fiber, fruit and vegetables. High total fat, red meat, omega-6 fatty acids, food additives, and the Western diet in general can have potential harmful effects. Complete enteral nutrition has been shown to be effective in remission of CD in children, but is often impractical. Other identified dietary interventions in IBD have not been well studied and have not been supported by a strong scientific evidence framework. But perhaps this does not really address the practical and most pertinent issue of how to counsel patients in daily practice. Thus, another identified diet that has not been discussed previously in this review may play an important role - the Mediterranean diet - an unrestricted diet with inclusion in the diet. include protective factors and exclude harmful dietary factors.
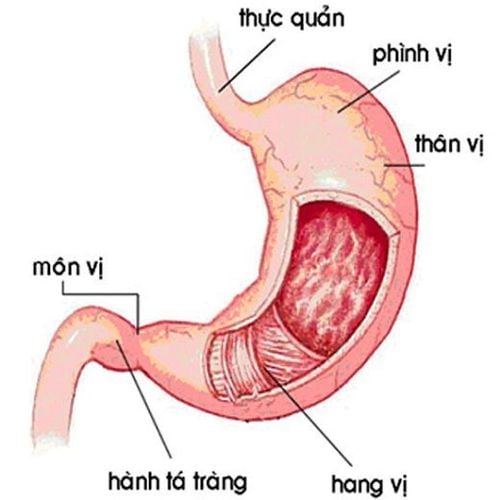
Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, diseases that cause chronic diarrhea, Crohn's disease, inflammatory bowel disease.. Along with that, at Vinmec Hospital, screening for stomach cancer and gastric polyps is done through gastroscopy with Olympus CV 190 endoscope, with NBI (Narrow Banding Imaging) function. narrow light frequency) results in clearer mucosal pathological analysis results than conventional endoscopy, detection of ulcerative colitis lesions, early gastrointestinal cancer lesions... Vinmec Hospital with modern facilities and equipment and a team of experienced experts who are always dedicated in medical examination and treatment, customers can be assured of gastroscopy and esophagogastroduodenoscopy services here. .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Siegel, CA. Refocusing IBD patient management: personalized, proactive, and patient-centered care. AmJ Gastroenterol. 2018;113:1440-1443. Malodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff, G et al. Increasing prevalence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142(1)46-54 e42. Shivasshankar R, Tremaine WJ, Harmsen WS, Loftus EV Jr. Incidence and prevalence of Crohn's disease and ulcerative colitis in Olmsted County, Minnesota from 1970 through 2010. Clin Gastroenterol Hepatol. 2017;15(6)857-863. Joseph D. Frasca, Adam S. Cheifetz, Diet and Inflammatory Bowel Disease: What is the Role? Practical gastroenterology • june 2019