This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
ERCP is a laparoscopic and lateral procedure that uses X-rays to view the pancreatic and bile ducts. ERCP is also used to remove gallstones or to take a small sample of tissue for analysis (biopsy).
1. Overview of endoscopic retrograde cholangiopancreatography (ERCP .)
1.1 What is ERCP? ERCP is the English acronym for “endoscopic retrograde cholangiopancreatography”, meaning endoscopic retrograde cholangiopancreatography. ERCP is a very useful procedure that can be used to diagnose and treat many different diseases, such as:
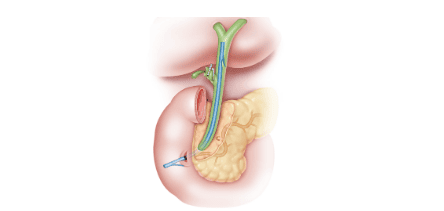
Gallstones Acute pancreatitis Chronic pancreatitis An endoscope is an optical tube with a diameter as small as approx. little finger and can be bent easily. To perform this technique, your doctor will use an endoscope that is passed through your mouth, into your esophagus, and down to your stomach and duodenum (the first part of your small intestine). The endoscope contains optical fibers that conduct light so the doctor can see inside the upper structures (gastrointestinal tract).
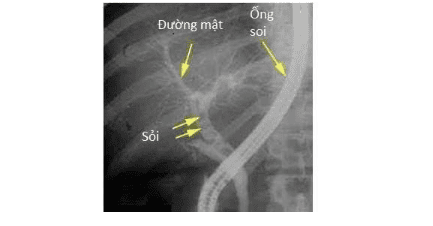
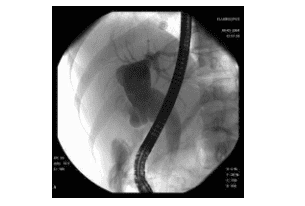
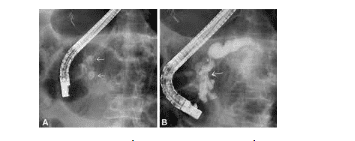
Pancreatic cholangiography is an X-ray method of the bile duct and pancreatic duct. These tubes are usually not visible on routine radiographs. However, if an X-ray contrast agent (contrast) is injected into the lumen, the X-ray film will show a clear picture of these tubes.
Normally, bile or pancreatic juice flows in these ducts toward the papilla (a special structure that forms where the common bile duct empties into the duodenum). When contrast is injected into the papilla through a plastic tube placed in the endoscope, the drug will travel up the pancreatic and bile ducts, so it is called “retrograde”. X-rays are taken at that moment to show the bile duct.
1.2 Biliary tract and nearby structures The liver is a digestive organ located in the upper right part of the abdomen. Bile, made by liver cells, moves into small tubes called bile ducts. These ducts merge to form the common bile duct. Bile flows continuously down the common bile duct and then flows through an opening called the "large papilla" to the duodenum.
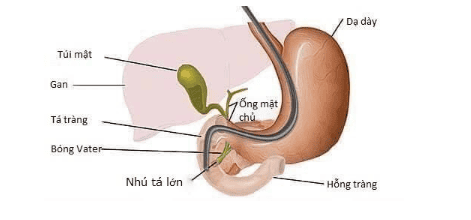
The gallbladder is located under the liver and also in the upper right side of the abdomen. It is like a pouch coming out of the common bile duct to help store bile between meals. The gallbladder contracts when you eat to empty the stored bile into the common bile duct. Bile passes through the remainder of the common bile duct and into the duodenum to help digest food, especially fats.
The pancreas is an organ that produces chemicals called pancreatic enzymes that help digest food. These enzymes drain into the pancreatic ducts, collect into the main pancreatic duct, and finally empty into the duodenum after passing through the papilla. The pancreas also produces some hormones such as insulin, glucagon, ... but they are secreted directly into the bloodstream.
1.3. How is ERCP performed? Your doctor may numb the back of your throat with a topical anesthetic spray. You are usually given a sedative into a vein in your arm. Sedatives make you drowsy and relaxed but do not induce sleep. This is not general anesthesia.
In the lying position on the bed, you will be asked by the doctor to swallow the end of the endoscope. Modern endoscopes are usually smaller than the index finger and quite easy to swallow. The doctor will gently push the scope down the esophagus, stomach, and into the duodenum.
The doctor will look at the inside of your stomach and duodenum through a monitor connected to the endoscope. Air is pumped into the stomach and duodenum through a channel in the endoscope, which helps to stretch the surface and make it easier to see. You may feel bloated and want to burp.
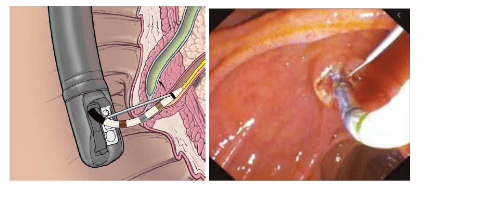
The endoscope also has a side channel for instruments to pass through, which is used by the doctor for a variety of purposes. Eg:
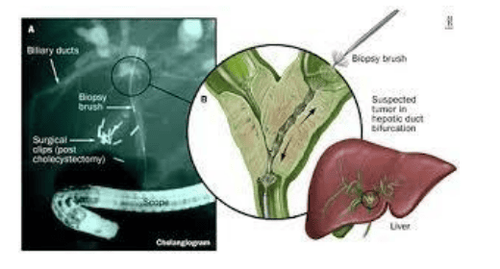
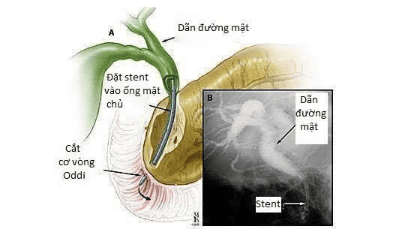
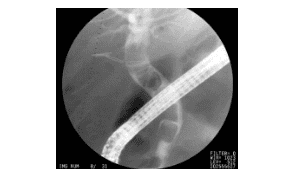
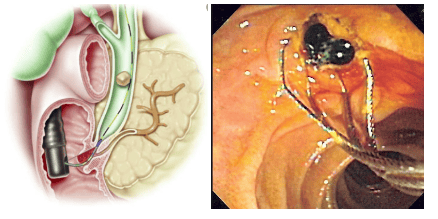
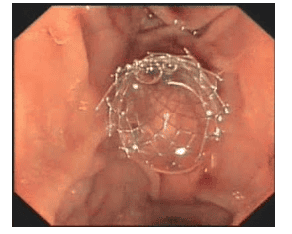
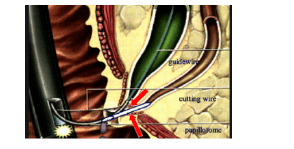
Inject the contrast agent into the bile duct or pancreatic duct. X-ray films are taken immediately afterwards to capture details in the tube. The injection can also show narrowing of the duct, stone stuck in the duct or tumor compressing the duct, etc. Biopsies are taken of the inner surface of the duodenum, stomach, bile duct and pancreatic duct near the papilla. The biopsy sample will be viewed under a microscope to look for abnormal tissues and cells. If the x-ray shows a gallstone stuck in the duct, the doctor will widen the papilla to allow the stone to drain into the duodenum. Stones can be collected in a “gab” or passed out with the stool. If X-rays show narrowing or blockage of the bile duct, the doctor may place a stent to widen the lumen. A stent is a small tube made of metal or plastic mesh. The stent allows bile to flow down the duodenum in a natural way. Stents can stay permanently in place without being felt by the patient. The endoscope is gently withdrawn at the end of the procedure. ERCP can be done in 30 minutes to 1 hour depending on the purpose of the test.
1.4. What to prepare for ERCP? You should be instructed by the hospital before having an ERCP. The instructions include:
Do not eat for several hours before the procedure. You are allowed to drink some water up to 2 hours before the test. Medications that need to be stopped before the procedure. Depending on the purpose of the procedure and you may need antibiotics. 1.5. What happens after ERCP? If ERCP is done just for X-rays, most people can go home after resting for a few hours. You should not drive, operate machinery, or drink alcohol for 24 hours after taking the sedative. If you go home on the day of the procedure, you will need someone to accompany you and stay with you for 24 hours, until the sedation wears off completely.
Most people can return to normal activities after 24 hours. Thanks to the sedation, most patients don't remember anything about the procedure. You may be required to stay in the hospital for a few days if ERCP is done to remove the stone or place a stent.
1.6. Does ERCP have any side effects or complications? Most ERCPs are performed safely and without problems. Some people have a mild sore throat a few days later. You may feel tired or drowsy for a few hours due to the sedation.
Less common complications include:
Injury to the intestines, bile ducts or pancreatic ducts caused by the endoscope. It can cause bleeding, infection and, rarely, perforation. If the following symptoms occur within 48 hours of ERCP, contact your doctor immediately: Abdominal pain – especially pain that is progressive, severe and of a nature other than heartburn, difficulty normal consumption. Fever. Difficulty breathing Vomiting/vomiting blood. Pancreatitis: This complication can be serious in some cases. The risk of complications is higher if you are in poor health. The benefits of the procedure should be weighed against the (albeit low) risk of complications. Tell your doctor if you think you may be pregnant. The ERCP procedure can still be performed in the case of pregnancy, after taking into account certain problems. Your doctor may recommend delaying ERCP or suggest another procedure.
2. Indications for endoscopic retrograde cholangiopancreatography
2.1. Indications for endoscopic retrograde cholangiopancreatography in diagnosis The doctor may appoint patients to perform endoscopic retrograde cholangiopancreatography to diagnose some diseases such as:
Jaundice of extrahepatic biliary obstruction of unknown cause Dilated biliary tract
Gallstones with dilatation of the common bile duct Bile duct tumors Oddi muscle dysfunction Dysplasia of the pancreatic duct
2.2 Treatment of Myotomy of Oddi: Indicated in cases of biliary obstruction due to inflammation of the stenosis of Oddi, dilatation of the common bile duct causing prolonged pain due to stenosis of Oddi.
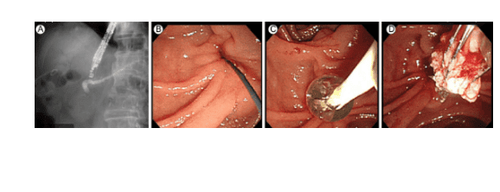
Collecting common bile duct stones: This is the most common indication of ERCP, with the help of lithotripsy devices such as mechanical lithotripsy, emergency lithotripsy, mother-child endoscope (SpyGlass), day More and more patients with gallstones have gallstones removed by endoscopic retrograde cholangiopancreatography without laparotomy.
Removal of pancreatic stones: In the past, to remove pancreatic stones, surgery was often required. However, complications of these surgeries are quite high, especially complications of pancreatitis. Today, with the development of technology and tools, it is possible to cut the pancreatic sphincter, remove pancreatic stones with a lower rate of complications.
Nasal biliary drainage Biliary stenting: Hilar cholangiocarcinoma: In the past, malignancies in the biliary tract caused obstruction, often requiring percutaneous transhepatic biliary drainage, with a certain number of adverse events. Today, with the advent of metal stents, with appropriate length, can be inserted into the right and left hepatic ducts, helping to decompress bile in the hepatic branches, increasing the patient's quality of life.
Cholangiocarcinoma outside the hilum of the liver when surgery is no longer possible. Benign biliary stricture
Large bile duct stones can not be removed immediately The common bile duct stone, but the patient's severe condition does not allow to remove the stone Biliary tract infection requiring drainage Pancreatic stenting.
Vinmec International General Hospital is a prestigious address in performing endoscopic retrograde cholangiopancreatography to diagnose and treat diseases of the biliary tract. Vinmec hospital system with modern facilities and equipment and a team of experienced experts who are always dedicated in medical examination and treatment, customers can rest assured with the retrograde cholangiopancreatoscopy service. at the hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
SEE MORE
Learn how to remove gallstones by ERCP at Vinmec Possible side effects or complications of endoscopic retrograde cholangiopancreatography Advantages of endoscopic retrograde cholangiopancreatography at Vinmec