This is an automatically translated article.
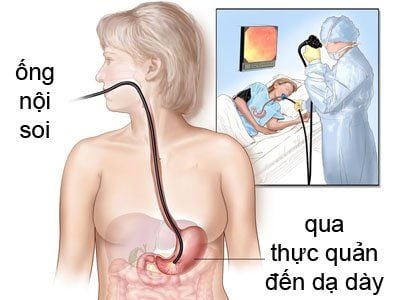
The article is written by Master - Doctor Mai Vien Phuong - Head of Gastrointestinal Endoscopy Unit - Department of Medical Examination and Internal Medicine - Vinmec Central Park International General Hospital.Acute pancreatitis after endoscopic retrograde cholangiopancreatitis (PEP) is a feared and potentially fatal complication that can be as high as 30% in high-risk patients. Pre-examination, intra-operative and post-examination measures are the key to clinical and technical success with the reduction of adverse events. Several studies have disputed this, however, many topics remain controversial, such as the efficacy of prophylactic drugs and the duration of amylase administration.
1. Prevention of acute pancreatitis after endoscopic retrograde cholangiopancreatitis
Certain measures can reduce the incidence of acute pancreatitis after endoscopic retrograde cholangiopancreatitis:(1) Adequate training and experience of endoscopists and assistants. (2) Use guidewire techniques to access the biliary tract. (3) Minimize the number of papillae openings. (4) Prophylactic pancreatic stenting in patients at high risk for acute pancreatitis after endoscopic retrograde cholangiopancreatitis. (5) Prophylactic pancreatic stenting in patients requiring guidewire placement in the pancreatic duct for biliary access (double guidewire technique). (6) Selective bile duct catheterization if pancreatic ductal evaluation is not required. (7) Minimize the volume of contrast injected into the pancreatic duct, if necessary. (8) Careful use of combustion current during sphincter ablation. (9) High-risk patients should undergo ERCP in specialized centers.
2. Effectiveness of preventive measures
Endoscopic technique:Endoscopic technique is an important factor in the development of acute pancreatitis following endoscopic retrograde cholangiopancreatitis. Selective catheterization with a hydrophilic guidewire should be performed, careful electrocautery should be used during sphincterotomy, and patients at high risk for acute pancreatitis after endoscopic retrograde cholangiopancreatitis should receive a stent. pancreatic duct prophylaxis.
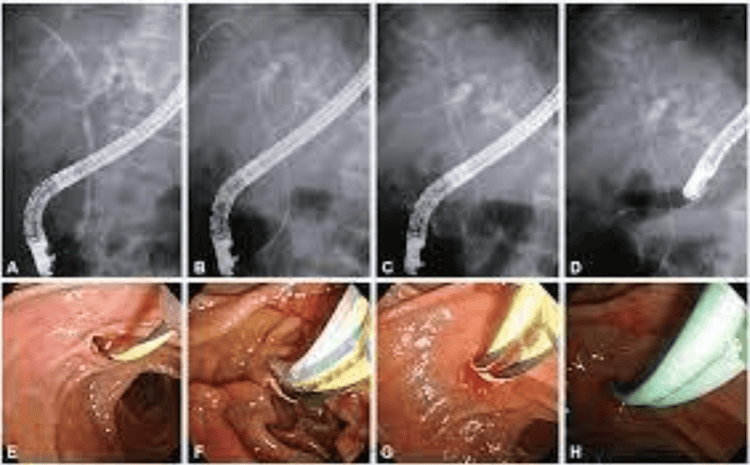
There are various tools as guidelines and can reduce the risk of acute pancreatitis after endoscopic retrograde cholangiopancreatitis as suggested by ASGE and ESGE. A system of randomized trials, evaluating a total of 3,450 patients, demonstrated that the guidewire technique tends to be superior to the contrast pump cannula technique. The success rate of papillary catheterization by guidewire is higher and the risk of acute pancreatitis after endoscopic retrograde cholangiopancreatitis is halved. In a multicenter randomized controlled trial (RCT), including 274 patients with duodenal papilloma, who had never undergone ERCP using guidewire papillary catheterization, in which the guide cord was inadvertently inserted into the main pancreatic duct. Patients were randomly selected to undergo either a two-guidewire or a single guidewire technique. Conversion to a double guidewire technique does not facilitate selective bile duct intubation and does not reduce the incidence of acute pancreatitis after endoscopic retrograde cholangiopancreatitis compared with a single guidewire technique. . However, double guidewire papillary catheterization is more effective in patients with malignant biliary atresia.
Electrocautery:
In a recent systematic review of 11 randomized studies involving 1,791 patients, it was found that performing electrocautery sphincterotomy in ablation mode alone resulted in higher bleeding rates. light blood is higher than that of endo and mixed. However, this method may have a lower incidence of pancreatitis. The unipolar regimen induces a higher incidence of pancreatitis than the bipolar regimen.
Pancreatic stenting:
Pancreatic stenting may be performed to prevent acute pancreatitis after endoscopic retrograde cholangiopancreatitis, mainly in high-risk patients. The authors recommend its use in patients undergoing pancreatic sphincterotomy. A comparison study of the main pancreatic duct when the use of a dual-pass technique is required, in patients with suspected sphincter of Oddi dysfunction and in patients undergoing anterior resection. The benefit may be thought to be related to the reduction in intraductal pressure of the ampulla of Vater. Studies have shown that, in exceptional situations, the passage of a pancreatic stent may be necessary to prevent the progression of pancreatitis following ERCP. This procedure must be performed 8 to 20 hours after the onset of acute pancreatitis following endoscopic retrograde cholangiopancreatitis. Pancreatic stents should be less than 5 cm short and small (5F) in diameter, plastic, and without a distal flange. Flangeless stents can lead to spontaneous migration to the gastrointestinal tract, occurring in 95% of cases within 10 days. If radiographs show evidence of stent persistence within 1 week, endoscopic removal of the stent should be performed. IV fluids:
ASGE guidelines recommend the use of intravenous fluids with Ringer lactate to reduce the risk of acute pancreatitis following endoscopic retrograde cholangiopancreatitis. In an RCT of 150 patients, the incidence of acute pancreatitis after endoscopic retrograde cholangiopancreatitis was lower in patients receiving intensive intravenous infusion compared with standard therapy. In patients with contraindications to rectal non-steroidal anti-inflammatory drugs (NSAIDs), who are not at risk for fluid overload and who have not had a pancreatic stent, the suggested alternative is aggressive hydration with oral solution. Ringer lactate solution (3 mL/kg/h during ERCP, 20 mL/kg bolus after ERCP and 3 mL/kg/h for 8 h after examination). Drug prevention:
Since 1977, more than 35 different drugs have been evaluated for the prevention of acute pancreatitis after endoscopic retrograde cholangiopancreatitis with mixed results. Includes:
NSAID rectal NSAID: ASGE and ESGE recommend NSAID use to reduce incidence and severity of acute pancreatitis following endoscopic retrograde cholangiopancreatitis (eg, 100 mg of indomethacin or diclofenac rectally) colon immediately before or after ERCP). A systematic review of 21 RCTs with a total of 6,854 patients found that rectal use of NSAIDs in all patients reduced the incidence of acute postoperative pancreatitis following endoscopic retrograde cholangitis and chronic pancreatitis. Mild pancreatitis is the only preventable outcome.
In this context, both diclofenac and indomethacin are considered effective. Rectal NSAIDs have also been indirectly compared with pancreatic ductal stenting. A meta-analysis showed that rectal NSAIDs are superior to pancreatic ductal stenting in preventing acute pancreatitis after endoscopic retrograde cholangiopancreatitis.
Non-rectal NSAIDs There are no data in the current literature to support the prophylactic use of any NSAID rectally or in combination with other agents. In a multicenter study of 430 patients, oral diclofenac (50 mg) before and after ERCP showed no benefit over placebo.
3. Other agents in the prevention of acute pancreatitis after endoscopic retrograde cholangiopancreatitis
There are several drugs that are potentially helpful in the prevention of acute pancreatitis after endoscopic retrograde cholangiopancreatitis, although some are difficult to access. Topical Adrenaline:A meta-analytical systematic review evaluating 6 randomized and 2 observational studies including 4,123 patients found that topical adrenaline did not confer any additional benefit at the end. In combination with rectal indomethacin for the prevention of acute pancreatitis after endoscopic retrograde cholangiopancreatitis in patients undergoing ERCP. However, topical adrenaline is associated with a lower risk of acute pancreatitis after endoscopic retrograde cholangiopancreatitis than placebo and may be considered if rectal indomethacin is not available or if the patient has any contraindications to the use of this drug. Nitrates:
In a review of 2,000 patients, the use of nitroglycerin was compared to placebo and it was found that the intervention group reduced the development of acute pancreatitis by 10% after endoscopic retrograde cholangiopancreatography. current. These data suggest that nitrates combined with rectal NSAIDs may provide more benefit than NSAIDs alone. In a randomized trial that included 886 patients on ERCP, the risk of acute pancreatitis following endoscopic retrograde cholangiopancreatitis was lower in patients treated with sublingual diclofenac suppositories and isosorbide dinitrate compared with patients treated with diclofenac suppositories and sublingual isosorbide dinitrate. patients using only diclofenac suppositories. Drugs that inhibit pancreatic secretion:
Somatostatin Somatostatin leads to a decrease in exocrine pancreatic secretion of both basal and stimulated origin. A meta-analysis including 9 studies concluded that somatostatin is not effective in preventing acute pancreatitis after endoscopic retrograde cholangiopancreatitis when administered for the short-term (<6 hours) or long-term (≥12) hour). Another meta-analysis, which included 11 RCTs with a total of 2,869 patients, found no benefit with somatostatin as a short-term infusion but showed a benefit with a single dose or a long-term infusion.
Octreotide Two systematic reviews with meta-analyses found no benefit of using octreotide for the prophylaxis of acute pancreatitis after endoscopic retrograde cholangiopancreatitis.
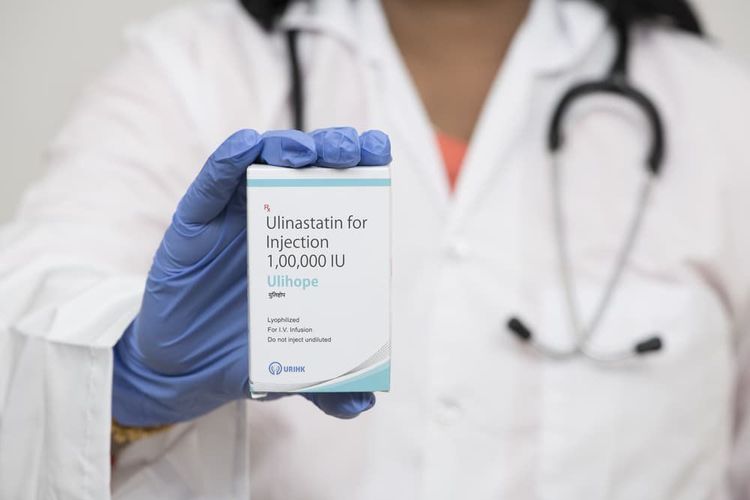
Inhibits Protease Activity: The most studied protease inhibitors include gabexate mesylate, nafamostat mesylate, and ulinastatin. Because the activation of proteolytic enzymes may contribute to acute pancreatitis after endoscopic retrograde cholangiopancreatography, protease inhibitors have been studied in the prevention of acute pancreatitis after endoscopic retrograde cholangiopancreatography. In a meta-analysis of 18 studies with 4,966 patients, there was a small benefit to using protease inhibitors.
Gabexate mesylate: Although controversial results were observed, a meta-analysis of five studies concluded that gabexate mesylate was not effective in reducing pancreatitis and pain after ERCP.
Nafamostat mesylate: Although controversial results have been observed, a meta-analysis including 7 RCTs with 2,956 patients showed a 53% reduction in the incidence of acute pancreatitis after endoscopic retrograde cholangiopancreatitis compared with patients. in the control group. Another meta-analysis including 26 studies, found that, unlike gabexate mesylate and ulinastatin, nafamostat mesylate and NSAIDs were associated with a reduced risk of acute pancreatitis following endoscopic retrograde cholangiopancreatography.
Ulinastatin: A systematic review with meta-analysis including 7 RCTs comparing ulinastatin with placebo or gabexate demonstrated a reduced risk of acute pancreatitis after endoscopic retrograde cholangiopancreatography in patients receiving ulinastatin.
4. Follow-up and care after ERCP
Many complications of ERCP are apparent within the first 6 hours after the procedure, and others may take days to manifest. The authors suggest the following recommendations:(1) Serum Amylase: Studies have shown that the 4-hour serum amylase level is a useful metric in predicting acute pancreatitis after cholecystoscopy. retrograde pancreas.
(2) Clinical monitoring: The immediate post-exam period is critical and patients must be monitored for signs and symptoms of adverse events.
(3) Diet: The authors recommend that patients fast for 6 to 12 hours after examination and discharge only after serum amylase results and clinical reassessment (eg, the patient is not abdominal pain).
5. Conclusion
Pancreatitis after ERCP is a scary, potentially fatal, and not entirely preventable complication. An accurate and early diagnosis is the turning point that determines the outcome of the disease. Pre-evaluation measures such as correct indication for the procedure, rectal NSAID use, and a trained endoscopist are necessary. During examination: Increase fluid, clear papillae accurately and quickly with correct technique and appropriate materials, use prophylactic pancreatic stent. After the procedure, maintaining fasting and proper amylase dosage is essential for the clinical and technical success of the procedure.Above is some information about prevention of acute pancreatitis after endoscopic retrograde cholangiopancreatitis. Please follow the website: Vinmec.com regularly to update many other useful news..
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Ribeiro IB, by Monte Junior ES, Miranda Neto AA, Proença IM, de Moura DTH, Minata MK, Ide E, dos Santos MEL, Luz GO, Matuguma SE, Cheng S, Baracat R, de Moura EGH. Pancreatitis after endoscopic retrograde cholangiopancreatography: A narrative review. World J Gastroenterol 2021; 27(20): 2495-2506 [DOI: 10.3748/wjg.v27.i20.2495]