This is an automatically translated article.
The article is written by MSc.BS Mai Vien Phuong - Gastroenterologist, Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Studies evaluating the effectiveness of the Spyglass cholangioscopy system have reported that visualization directly improves the accuracy of cholangioscopy results and has a positive good predictive value in the evaluation of patients. have symptoms of biliary obstruction of unknown origin.
1.BACKGROUND ERCP is a very useful procedure that can be used to diagnose and treat many different diseases of the biliary tract and pancreas. However, for tumors inside the common bile duct, liver hilar tumor, to definitively diagnose this pathology, is still a dilemma, because it is not possible to see directly, it is not possible to take tissue samples inside the biliary tree. Perform histopathological examination to determine whether the tumor is benign or malignant.
Most of the previously diagnosed cholangiocarcinomas were diagnosed through the C-Arm screen of the radiograph. Another problem is that when performing ERCP, for large stones, it is often necessary to use a mechanical lithotripsy, or switch to a common bile duct stone removal surgery, and ERCP cannot completely remove the stones. stones in the right and left hepatic ducts.
Learn more about ERCP: Endoscopic retrograde cholangiopancreatography (ERCP): What you need to know
With advancements in technology, the advent of SpyGlass (transoral cholangioscopy) has solved these problems. this.
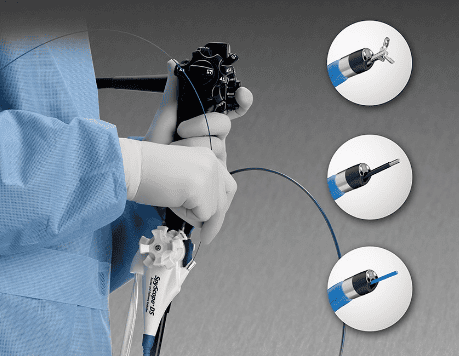
2. SpyGlass Transoral Cholangioscopy System Peroral cholangioscopy has also been evaluated as an effective tool for the evaluation of pancreatic ducts. A study by Yamaguchi et al. reported an improved ability to diagnose papillary mucinous tumors of the pancreas due to pancreatic adenocarcinoma using a mother-infant cholecystoscope. Importantly, this study also concluded that there is no cytological value with pancreatic juice in the diagnosis of pancreatic carcinoma. Studies evaluating the effectiveness of the Spyglass cholangioscopy system have reported that visualization directly improves the accuracy of cholangioscopy results and has a positive good predictive value in the evaluation of patients with symptoms of biliary obstruction of unspecified origin. Endoscopy-guided biliary tract biopsy can be performed successfully in 89% of cases. An unexpected benefit of endoscopic cholangiography is that it has revealed a weakness previously not assessed in ERCP in the evaluation and diagnosis of choledocholithiasis. Parsi et al were able to diagnose at least 29% of ERCP missed gallstones by performing endoscopic cholangiography, leading them to conclude that the rate of stone loss on ERCP may be higher than previously thought. this. Studies have reported a 92% success rate in the treatment of cholangiolithiasis using electrohydraulic lithotripsy and laser lithotripsy. Moon et al. reported excellent success with electrohydraulic or laser lithotripsy using an ultrathin cholecystoscope.

In patients with difficult to treat stones, Arya et al described the technique of transoral cholangiography with electrohydraulic lithotripsy in 94 patients who reported 96% fragmentation and 90% stone clearance rates. . Furthermore, Hui et al demonstrated significantly less cholangitis and a reduced mortality rate with lithotripsy-guided endoscopic cholangiography compared with biliary stenting alone in elderly patients. . Many other studies report similar success rates in the treatment of gallstones using transoral cholangioscopy and electrohydraulic or laser therapy. Therefore, when performed by an experienced and trained person, transoral cholangioscopy can be a safe and highly effective technique for difficult-to-treat gallstones.

3. Contraindications Contraindications for Cholangioscopy include the following:
Any condition that precludes the patient from undergoing endoscopic surgery Acute pancreatitis ruled out by gallstones Coagulation disorder with a risk high bleeding risk Changes in the anatomy of the gastrointestinal tract that prevent access to the second part of the duodenum (eg, Roux-en-Y gastrointestinal surgery) 4. Technique Plan for the procedure Because the biopsy tissue sample from the SpyGlass scanner is very small, it is necessary to notify the pathology department, warning when the biopsy sample from the cholangioscopy may be small. When the amount of tissue sample obtained during cholangioscopy is very small, this communication will ensure optimal handling of the precious specimen.
Prevention of complications SpyGlass cholangioscopy involves vital manipulation of the bile ducts. Prophylactic antibiotics are usually given before surgery, with Levofloxacin, ampicillin, and gentamicin being the most commonly used antibiotics. Warnings are there to confirm that coagulation parameters are normal prior to the procedure to prevent the risk of bleeding.
5. Patient care before and after the procedure
Patient Education / Sign Procedure Consent: Procedures performed and risks associated with anesthesia and procedure should be explained.5.1 Patient Instruction Patients should be instructed to fast overnight prior to surgery.
5.2 Pre-procedure planning This procedure should be explained to the support staff, to the endoscopic assistant nurses.
All necessary equipment should be checked before starting the procedure
Prophylactic antibiotics are usually given 30 minutes before surgery.
5.3 Device Two operating systems: Mother-child endoscope and mini-endoscope
These endoscopes use a large “mother” endoscope for duodenoscopy and then use an endoscope” baby” is smaller to pass through the surgical channel into the bile duct. When introduced, it was a revolutionary technology that successfully provided imaging of the bile ducts and pancreatic ducts. It also offers excellent diagnostic and therapeutic potential in the management of biliary tract disorders.
The first “mother-child” cholangioscopy system has many limitations. They are fragile and cumbersome, require two endoscopic surgeons, are limited to bidirectional endoscopic direction, lack working channels, are less widely available, and require high expertise, and have high maintenance costs. high maintenance.
Mini endoscope developed later. They are introduced into the bile duct through a standard duodenoscope. The previous version was fragile, had no reflector at the nose, and lacked working channels.
The larger mini-endoscope was later developed to overcome the earlier limitations of the smaller tube. Advantages include the possibility of treatment from instrumentation channels, but they are limited by the absence of separate air and water channels.
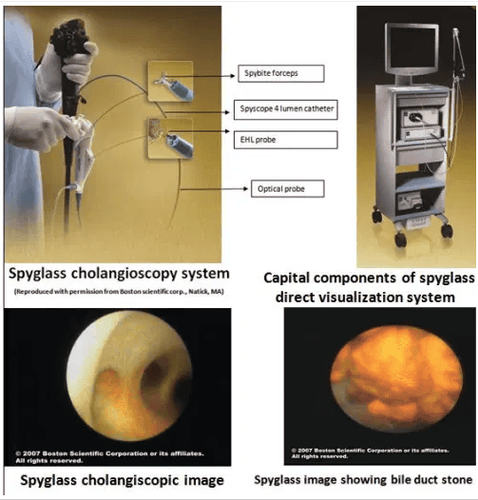
System components include:
Light source and power cable (300-W high intensity white light) Camera and image processing system (camera autoshutter with color image sensor) Eyes optical coupler interface with probe and camera Irrigation system Vedeo display Regarding the procedure system, the standard ERCP bronchoscope system has a 10-F outer diameter test channel, a 230 cm Spyscope wire and Outer diameter of the 10 F-consists of 4 small channels: one for the Spyglass probes, one for the Spybite biopsy forceps, and the hydroelectric lithotripsy system or laser probe. Two water pump channels exit at the end of the water channel of the duct.

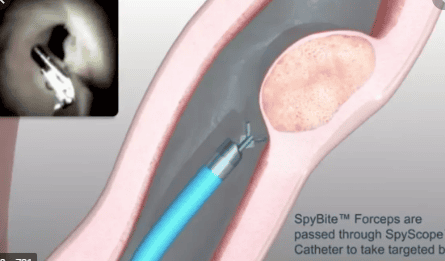
The Spyglass fiber optic probe is a multi-use device with a length of 231 cm that performs light to the bile ducts and endoscopic fiber optic imaging. It consists of a 6000-pixel image, surrounded by a beam that transmits approximately 225 light. A lens connected at the far end of the image bundle captures a 70-degree angle. The Spybite biopsy forceps are a single-use device measuring 286-cm in length. The clamps were inserted into the biliary tract through the 1.2 mm working channels of the Spyscope catheter. The jaws are designed with a central edge and have an outer diameter of 1 mm for the collection of small target biopsies by direct visualization. The Spyglass system is compatible with a hydroelectric lithotripsy system and laser probes inserted through the working channel of the Spyscope catheter.
6. Patient Preparation Anesthesia Cholangioscopy is a time-consuming and labor-intensive procedure. Patients are deeply sedated with midazolam/fentanyl by an anesthesiologist during a commonly used procedure. In some cases, general anesthesia may be required to perform the procedure. Protecting the airways is an important concern during a protracted procedure such as cholangioscopy, which further emphasizes the need for the anesthesiologist. The patient should be continuously monitored for blood pressure, heart rate, heart rate, respiratory rate, and oxygen throughout the procedure. Positioning The patient is usually placed in a prone position with the head tilted to the right.
Complications Complications associated with cholangioscopy range from relatively mild to life-threatening complications, including the following:
Cholangitis (most common complication) Infection Abdominal pain Lower pancreatitis blood pressure Nausea Liver abscess Bile duct perforation (from the lead) Elevated amylase and lipase without clinical pancreatitis Inflammation Syndrome Technique Cholangioscopy using the Spyglass cholangioscopy system can be performed by a single endoscopist. The duodenoscope along with the Spyglass cholangioscopy system is performed by the hand of an endoscopist. The remaining hand of the endoscopist is used the main camera of the duodenal endoscope system and Spyglass. This procedure is done in conjunction with ERCP. The Spyglass machine directly probes into the optical channels of the Spyglass catheter. Under direct view, the duodenoscope is passed through the oral cavity and pharynx. The duodenoscope is then passed through the esophagus and stomach to reach the second segment of the duodenum to visualize the ampulla of Vater and the papilla. Selective passage into the biliary tract is performed. A guide wire is inserted and positioned in the bile duct (or pancreatic duct) using a fluoroscopy (C-Arm) x-ray machine. Sphincterotomy of Oddi is often performed. The Spyscope, together with the optical probe, is inserted into the duodenal endoscope together as a unit and into the bile duct for direct visualization of the inside of the pancreatic biliary tract. Once inside the common bile ducts, Spyglass's path is examined under a fluorescein (X-ray) screen. Once the Spyscope catheter is positioned in the common bile duct, the lead is removed. Optical probes are placed at the tip of the Spyglass catheter. Direct visualization of the bile ducts was performed by repeatedly advancing and withdrawing the Spyscope catheter in the bile duct.
If a suspected lesion is found in the bile ducts, Spybite clamps (alkaline biopsies) are inserted through the operating channels to obtain small targeted biopsies. If gallstones are found, Spyglass directs hydrodynamic lithotripsy or laser lithotripsy is performed. Water during manipulation from the bile ducts is drained through water channels installed in the Spyscope catheter and exits at the catheter tip. This will clear debris in the bile ducts and provide better visualization during the procedure. The lack of a suction port is a drawback of this system, but assisting with the suction problem can be achieved by attaching a syringe to the operating channel. After the procedure is completed, the patient is usually not allowed to eat or drink until the next day. Perform sphincterotomy of Oddi Sphincterotomy. A cholangiogram is then performed and a wire is placed in the biliary system. The cholangioscope is inserted into the working channels of the duodenoscope to cannulate the common bile duct. Once the cholangioscope enters the lumen of the common bile duct, the guidewire can be removed. The working channels available in the endoscope are used for diagnostic and interventional therapy. Small biopsies can be obtained by inserting forceps through the working channels of the cholangioscope. Electrohydraulic lithotripsy or laser lithotripsy can also be performed through the working channels of the biliaryoscope. Direct cholangioscopy Direct cholangioscopy is a relatively new technique with limited information available. This is a technically difficult procedure that requires resection of the larger sphincter of Oddi and dilated bile ducts, but the image quality is superior. This trick can be done by using a guide wire or ball support trick. A standard therapeutic duodenoscope is inserted into the second part of the duodenum, similar to the previously mentioned method for cholangioscopy. A guide wire is then inserted into the bile ducts under a fluorescein screen, after which the duodenoscope is removed, leaving the leads in the bile duct. An ultrathin endoscope is then inserted into the biliary tract following the guide and guidance of the fluorescein screen. If a balloon-assisted method is used, a balloon is inserted and inflated in the common hepatic duct. This is used as an anchor to advance the ultrathin endoscope into the bile duct.
Conclusion: With the introduction of the SpyGlass system, it has opened up new treatment prospects for patients with biliary tract disease, reducing invasive interventions, bringing better quality of life for patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.