This is an automatically translated article.
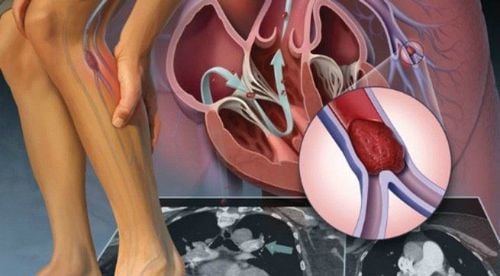
The article was written by a Doctor of Hematology - Blood Transfusion - Laboratory Department - Vinmec Ha Long International Hospital.Blood transfusion today has become a common treatment to maintain life for patients with anemia, or in surgical support... But few people know that in order to be able to carry out the dream job. Seemingly normal, scientists in the past had to spend a lot of effort to conduct risky experiments to find out the principle of blood transfusion. The story of the birth of Hematology and Blood Transfusion is associated with thrilling experiments that have caused the death of many people.
The idea of blood transfusion first appeared around the middle of the 17th century by the medical names of this period and was recorded by a man named Stefano Infessura.
According to the above record, in 1492, when Pope Innocent VIII fell ill and fell into a coma, the blood of 3 boys was used by the medical gods to give the pope orally. At that time, people did not fully understand the process of blood circulation and the principle of blood transfusion, but only considered blood as an important factor to nourish the human body. The boys selected for blood collection were only 10 years old, after having had a significant amount of blood taken to serve the pope, had to die from blood loss. The deaths of the first humans associated with this blood transfusion experiment have been recorded in the history of Medicine as the first accidents related to the Hematology and Blood Transfusion industry of mankind.
Until 1616, the English physiologist William Harvey discovered the circulation of blood and that it was the heart that was responsible for pushing blood to nourish the parts of the body. This was considered a revolution because at that time, the views of ancient medical scientists still played a dominant role. They believe that blood is made by the liver, warmed by the heart as it passes from the right ventricle to the left ventricle. This discovery revived the idea of blood transfusion to revive and strengthen people in the medical world. Many doctors have tried injecting blood into animals and they have been successful.
In 1660, experiments on blood transfusions conducted on animals and between animals and humans continued to cause loss of life, but it also helped experts in the field better understand the cause theory of blood transfusion, and at the same time bring the branch of Hematology and Blood Transfusion towards perfection. After William Harvey's discovery about the circulation of blood in the body, surgeons in London (England) and Paris (France) began to conduct experiments on transferring blood from calves and sheep to animals. dogs, or blood transfusions from dogs to cows, or from goats to horses... But the most remarkable experiment was the experimental blood transfusion from sheep to humans. The person chosen to participate in this experiment to receive blood from sheep was an Englishman named Arthur Coga. The trial was successful, according to scientists at the time, because at least Arthur Coga's patient recovered for some time before dying.

Hình ảnh bác sĩ Jean Baptise Denis truyền máu cừu cho người

Hình ảnh bác sĩ Jean Baptise Denis truyền máu cừu cho người
Success after 150 years of waiting
Before the real success of human blood transfusion, the first successful blood transfusion experiment was conducted by an English doctor named Richard Lower in 1665. He was also the one who developed the blood transfusion. invented the first rudimentary blood transfusion kit in history. But his success was only achieved when conducting blood transfusions on dogs.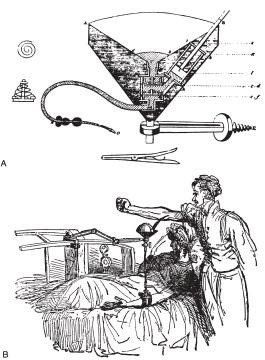
: Bác sĩ Richard Lower phát minh ra dụng cụ truyền máu (1665)
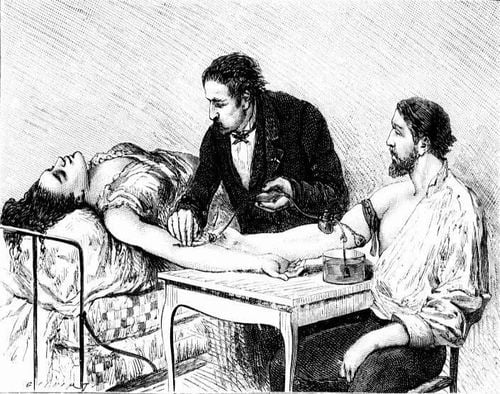
Bác sĩ James Blundell truyền máu chồng cho một sản phụ
After the success of Dr. Blundell, the field of Hematology and Blood Transfusion has really developed and achieved successive successes. In 1840, at the George College of Medicine, London (UK), with the help of Dr. Blundell, a student named Samuel Armstrong Lane conducted a blood transfusion to save the life of a patient suffering from hemophilia. bronze . But, the success rate of blood transfusions is very low and depends on great luck.
But it was only in 1901, when Austrian scientist Karl Landsteiner discovered blood types, and is considered an important discovery in science, because it helped scientists do the work that they have been trying for two centuries, and at the same time paved the way for the development of hematology and blood transfusion. At this point, people realized that: In fact, the failure of previous experiments was due to the fact that the blood transfused into the patient's body was not received and eliminated due to the wrong blood type. And getting the right blood type is an extremely important thing in blood transfusion. Blood transfusions have become much safer, and the risk of death in blood transfusions is almost zero.
In 1916, the first blood bank was established in France by the scientist Oswald Hope Robertson.
To the twentieth century: The mysterious problem of blood transfusion has been opened
The most valuable and most beneficial scientific work in blood transfusion is the invention of red blood cell and blood group antigens by the Austrian doctor Karl Landsteiner (1868 - 1943).In 1900, while studying the relationship between red blood cells and human serum, Landsteiner noticed that the serum of some people causes agglutination of the RBCs of some people, but the RBCs of others do not. .
After thousands of experiments, in 1901 he concluded that the serum of a group of people (symbol A) causes agglutination of the red blood cells of another group (symbol B), but does not cause agglutination of the red blood cells of the same person. group A; The erythrocytes of group A people are agglutinated by group B's serum. The 3rd group's serum (denoted by C) causes agglutination of the red blood cells of both group A and B, and the erythrocytes of group C. was not agglutinated by the sera of group A and B.
From there he built 3 groups of people with their own agglutination characteristics and called them group A, B, C (group C later called O). That is:
People with red blood cells A have no agglutinin A (group A); People with B red blood cells do not have B agglutinin (group B); People with both A and B agglutination in the serum have red blood cells that do not have A and B antigens (group O). A year later (1902) Decastello demonstrated the fourth group, his red blood cells did not have A and B agglutination, but had both A and B antigens (group AB). Thus, Landsteiner and his students found four blood groups A, B, AB and O, called the ABO blood group system for short. From here he came up with the rules of blood transfusion of the ABO blood group system.
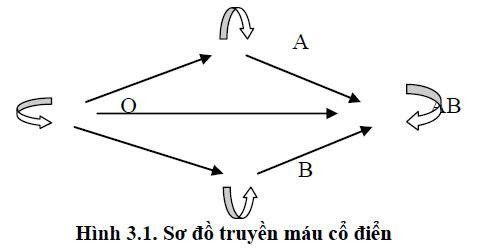
Sơ đồ truyền máu

Bác sĩ Karl Landsteiner (1868 - 1943)
From 1927 - 1947, Landsteiner and his students discovered more blood group systems besides ABO, which are M, N, p... and in 1940 discovered the Rh (Rhesus) system. At the same time, the author has experimentally created anti-Rh antibodies by sensitizing monkey erythrocytes to rabbits, and found that rabbit serum causes agglutination of > 85% of human erythrocytes, this group has Rh antigens, called Rh positive. (Rh+); The rest (non-reactive) is a group of red blood cells that do not have Rh antigens, called Rh negative (Rhr).
At the end of life (about 1940-1950) Landsteiner and his students discovered the inheritance of blood groups between father, mother and child. At the same time, through many experiments, he came to the conclusion: the M, N, p and Rh systems do not have natural antibodies, antibodies against this antigen can only be obtained from pregnant mothers many times, or the recipient blood transfusion multiple times. So today we call them immune antibodies, and ABO blood group specific antibodies are natural antibodies, they are available from embryo development.
At the same time, Landsteiner and Weiner harvested rabbit serum sensitized by Rhesus monkey erythrocytes (Rh+) and compared it with the serum of patients causing non-ABO transfusion reactions. +) and was similar to negative for anti-rabbit monkey erythrocytes (Rhesus). This is the basis for the authors to discuss the possibility of using Rh immune globulin to protect hemolytic disease in neonates. This is a new progress, considered as the "work of the century" in the protection of human health.
Anticoagulation in blood transfusion is big work
Due to the increasing demand for blood, in order to preserve and store blood for a long time to be available for emergency and treatment of patients, preservatives are required. Braxton (1869) introduced Phosphate antifreeze. Then Weil (1915) introduced Citrate solution, which was used during World War I. By 1936 the Citrate solution was replaced by the Acid-Citrate-Dextrose (ACD) solution.During the Second World War, Loutit (1943) developed the ACD (Acide-Citrate-Dextrose) formula to anticoagulant large volumes of blood and blood can be stored at cold temperatures for longer days, the author used rate of 70 mL of anticoagulant ACD 450 mL of blood. This ratio was used throughout the Second World War. Later, in the l970s, due to the need for longer-term blood preservation, the new anticoagulant CPD (Citrate-Phosphate-Dextrose) replaced ACD.
By the end of the twentieth century, a longer-term blood preservation solution (35-42 days) CPD-A (Citrate- Phosphate-Dextrose-Adenine) was used. Thus, the development of anticoagulants has contributed to safer blood transfusion and the development of blood banks with the ability to store blood: CPD keeps blood for 21 days; CPD-A1 can be stored for 35 - 42 days at 2 - 60C.
Up to now, anticoagulants and the ability to nourish red blood cells and platelets of anticoagulants are still an interesting issue for researchers in the field of blood transfusion safety.

Túi dẻo chứa chất chống đông CPD-A1 đang được sử dụng hiện nay
Kỹ thuật truyền máu ra đời từ Thế chiến thứ nhất và trở thành một trụ cột của y học cho tới tận bây giờ
A system of modern and advanced medical equipment, possessing many of the best machines in the world, helping to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of doctors the most effective. The hospital space is designed according to 5-star hotel standards, giving patients comfort, friendliness and peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
REFERENCESDepartment of Hematology-Blood Transfusion, Hanoi Medical University (2014). Lecture on Hematology-Blood Transfusion (Graduate). Medical Publisher. Website of the National Institute of Hematology and Blood Transfusion: nihbt.org.vn Website of the Ho Chi Minh City Blood Transfusion and Hematology Hospital: bthh.org.vn Source: - THE HISTORY OF BLOOD TRANSFUSION AND BLOOD TRANSFUSION MEDICINE. bloodbook.com/trans-history.html.
- The History of Blood Banking.