This is an automatically translated article.
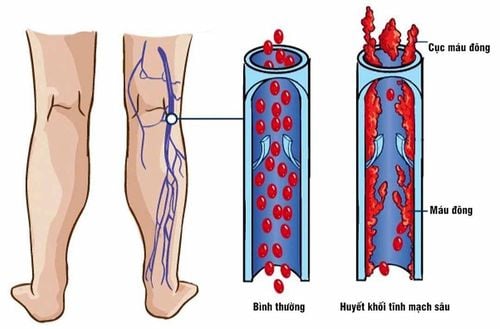
Diagnosis of lower extremity deep vein thrombosis is based on clinical symptoms of the patient, exploiting predisposing risk factors, assessing clinical risk of DVT to select methods. testing, diagnostic testing.1. Symptoms of lower extremity venous thrombosis
Symptoms of deep vein thrombosis of the lower extremities are pain and swelling in the legs. However, in certain patients, the history may be asymptomatic if the thrombus does not obstruct venous outflow.1.1 Leg edema Leg edema is the most specific symptom of deep vein thrombosis of the lower extremities. Thrombosis involving the bifurcation of the pelvis, iliac vein or vena cava, will cause leg edema.
Partial obstruction of the superior vena cava often causes mild bilateral leg edema. Massive edema of the lower extremities combined with cyanosis and ischemia of the leg is very rare.
1.2 Leg pain Hypersensitivity is also seen in 75% of patients but also in 50% of patients without objectively confirmed DVT. When it comes to pain, it's usually localized to the calf muscles or along the deep veins in the mid-thigh.
Also, lower extremity deep vein thrombosis pain does not usually correlate with the size, location, or extent of the thrombus. Occasionally, hot skin or erythema over the area of the thrombus is noted.
1.3 Thrombophlebitis Superficial thrombophlebitis can also be a manifestation of symptomatic deep vein thrombosis of the lower extremities. A segment of subcutaneous vein is taut, tender to the touch.
Approximately 1⁄2 of the patients have superficial thrombophlebitis without associated varicose veins and no other obvious cause (eg, intravenous catheter, intravenous drug abuse, tissue trauma). soft) is associated with deep vein thrombosis. Even patients with superficial thrombophlebitis extending to the omental junction have a higher risk of DVT.
In addition, the patient also had venous thrombosis with symptoms of lower extremity discolouration. The most common abnormal color is purple-red due to varicose veins and occlusion. In rare cases, cyanosis of the legs due to complete venous obstruction, initially described as blue, is later accompanied by marked edema, pain, and cyanosis; sometimes there are additional bleeding spots.
Without treatment, half of patients with recurrent deep vein thrombosis develop symptoms within 3 months. At the same time, after stopping anticoagulation, the recurrence rate is also up to 5-15% per year.
Recurrence of deep vein thrombosis of the lower extremities is similar to the first, with pain and edema. However, the diagnosis of DVT can be difficult, i.e. distinguishing acute from chronic thrombosis).
In addition, recurrent cases will also increase the risk of developing post-thrombotic syndrome.

Huyết khối tĩnh mạch sâu chi dưới triệu chứng phổ biến là cảm giác đau ở chân
2. How is deep vein thrombosis diagnosed?
Because symptomatic cases of deep vein thrombosis of the lower extremities have low sensitivity and specificity, this diagnosis requires a combination of laboratory tests, especially evidence of thrombosis on imaging. Routine blood tests that can help physicians stratify patients for DVT risk include: D-dimer test; antithrombin III, NT-proBNP and C-reactive protein levels; erythrocyte sedimentation rate.To confirm the diagnosis, clinical prediction rules should first be used to estimate the probability of experiencing a venous thrombosis. In which, the Wells score for deep vein thrombosis as well as pulmonary embolism is commonly used.
Second, in patients with a high probability or pre-existing disease, a highly sensitive D-dimer is indicated. A negative result indicates a low likelihood of disease.
Third, in patients with a moderate to high likelihood of DVT of the lower extremities, the indication for DVT of the lower extremities should be initiated initially.
However, if the patient suspects the possibility of deep vein thrombosis of the lower extremities causing pulmonary embolism, imaging should be confirmed. Options now include ventilation-perfusion (V/Q) tomography, multi-probe torsion computed tomography (CT), and pulmonary angiography. Of these, CT alone may not be sensitive enough to rule out pulmonary embolism.
In addition, tests of coagulation function should also be ordered to support the diagnosis of venous thromboembolism, including: Quantification of protein S, protein C, antithrombin III, factor V Leiden, prothrombin 20210 mutation A, antiphospholipid antibodies and homocysteine levels. The deficiency of these factors as well as the abnormal presence produce an inappropriate coagulation state. However, these are very rare causes of deep vein thrombosis.

Siêu âm huyết khối tĩnh mạch sâu chi dưới để phát hiện và điều trị sớm
In summary, lower extremity deep vein thrombosis symptoms may include edema, leg pain, increased sensitivity, hot or erythematous skin, and skin discoloration over the area where the thrombus is located. On physical examination, the doctor may detect calf pain when flexing the instep or palpating an inflamed vein.
However, it is recommended that deep vein thrombosis of the lower extremities be confirmed diagnostically on the basis of imaging evidence, depending on the risk class, along with screening for coagulation function as a means of etiology.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.