This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Despite significant advances in the medical management of inflammatory bowel disease in recent years, many patients will require surgery. Many of these situations are elective or subacute surgery that may be postponed for days or weeks in some patients with confirmed COVID-19. However, there may be emergencies such as perforation of the colon, acute severe colitis, uncontrolled bleeding, surgery in these cases cannot be postponed but must be treated promptly.
At the height of the pandemic, one of the side effects was that elective surgeries were canceled or temporarily suspended. Elective surgeries for inflammatory bowel disease cannot be delayed for too long when they are strictly indicated, mainly because of the increased morbidity due to impaired patient status (eg, steroids and malnutrition maintenance). Surgical treatment of these patients with inflammatory bowel disease should not be delayed, regardless of their COVID-19 status.
1. Conducting emergency surgeries during a pandemic like COVID-19 is a challenge
Conducting emergency surgeries during a pandemic like COVID-19 is a challenge for inflammatory bowel surgeons and the entire hospital infrastructure. The available information about COVID-19 and the potential for aerosol and droplet contamination led to the need for modifications to perform successful surgery, reduce the risk of hospital facility contamination, and protect medical staff and patient. It is important to protect all surgical teams (e.g. masks, glasses, visors, and surgical caps) to prevent transmission of COVID-19 when they are performing surgery on patients with inflammatory bowel disease with COVID -19 suspected or confirmed and protect the patient to prevent COVID-19.
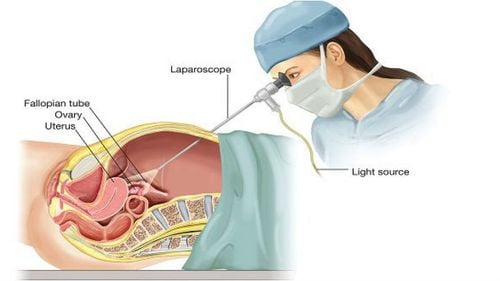
2. Concerns about minimally invasive surgery
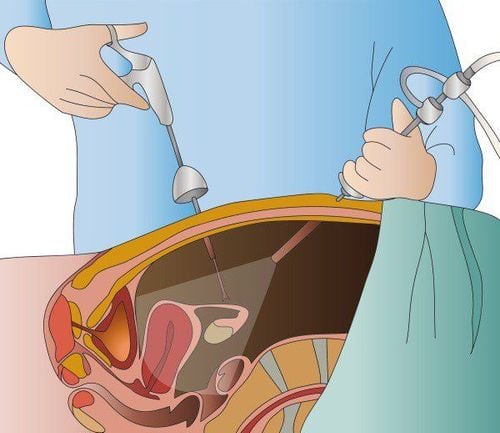
There is concern among surgeons with minimally invasive techniques (eg, laparoscopy and robotic surgery) due to the possible risk of transmission of the COVID-19 virus with the creation of pneumoperitoneum. However, minimally invasive surgery (MIS), including laparoscopic surgery, is feasible and safe in inflammatory bowel disease and has many advantages, such as reduced hospital stay, less pain, less trauma, less effect on respiratory motility, reduced morbidity and faster postoperative recovery There is little evidence of virus transmission through endoscopic or open approaches. As shown by Somashekhar et al., the risk of infection by COVID-19 to the healthcare team during minimally invasive surgery (laparoscopic or robotic) is considered low. Therefore, in inflammatory bowel disease, we should not postpone surgery, even if considered "option", due to the COVID-19 pandemic. Therefore, the care that must be followed by the surgical, nursing, and anesthesiological teams must be standardized at the referring hospital and replicated to other health services referenced in the surgical treatment of patients. enteritis.

3. Precautions to avoid contamination of the surgical team
Precautions to avoid contamination of the surgical team are described in several studies published during the pandemic and include care for airway management during anesthesia and specific care when abdominal endoscopy. There seems to be consensus in the literature that intubation and extubation are high-risk procedures for medical professionals and that the maximum amount of PPE is required. However, there is little evidence about the real risk of contamination by health care professionals during laparoscopy, as well as operating room pressure (OR), surgical smoke, tissue extraction, or CO2 discharge. If surgery is deemed necessary, the surgeon must minimize the risk of exposure to the virus, involve a minimum number of medical professionals, and shorten the working hours of the surgeons. OR. As noted, there are no absolute contraindications to minimally invasive surgery; however, PPE is suitable for the OR team and the filter/exhaust system is recommended unanimously.
4. Some techniques to make minimally invasive surgery safer
If safety measures are lacking to allow safe laparoscopy, open surgery should be considered. However, previous studies have shown that aerosols of bacteria and viruses can be detected during both open and laparoscopic surgery, the latter of which should also be a surgical aspirator/aspirator. used in open processes. Power tools and power devices should be used at the lowest power levels to prevent the generation of too much aerosols and fumes There are a few tips and tricks to make minimally invasive surgery safer during the COVID-19 pandemic, such as avoiding the creation of leaks to escape smoke, using a closed exhaust system; Using non-leakage trocars such as balloon trocars, total pleural aspiration prior to surgical specimen collection at the end of procedure prior to trocars collection, or prior to conversion to open surgery. Hospitals must prepare specific internal procedures and arrange for adequate training of relevant staff.
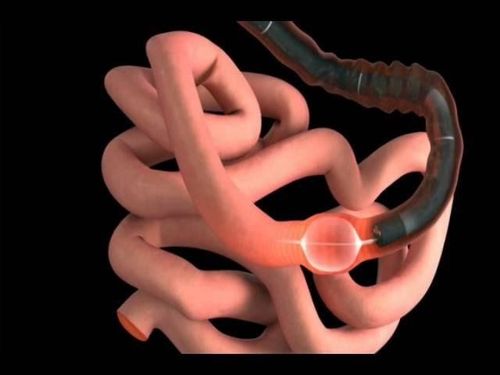
All surgical teams must strictly follow all rules regarding COVID-19 infection If possible, postpone elective surgery and consider screening all surgical patients for COVID-19 with an RT-PCR swab or a chest CT or chest X-ray. In urgent surgeries (<24 hours), such as perianal abscess, bowel perforation, megacolon (toxic megacolon), surgery must be performed immediately and all patients must be treated as if they were positive for COVID-19. All surgical teams must strictly follow all rules regarding COVID-19 infection. The same rules apply to patients in emergency situations (<72 h), such as bowel obstruction (non-ischemic). Elective surgeries (up to 4 weeks to 3 months) must take an individualized approach. However, surgical resection in patients with chronic refractory ulcerative colitis or dysplasia and colorectal cancer in ulcerative colitis should be converted to surgery, preferably before this stage, to The initial clinical condition did not get worse. It is important to emphasize that all known or suspected COVID-19 positive patients requiring surgical intervention should be treated until proven otherwise to minimize the spread of infection. In addition, whenever possible, dedicate ORs specifically to patients with COVID-19. Create negative pressure in room one as they are considered ideal; however, most ORs operate at positive pressure and therefore their use is permitted. An air exchange rate ≥25 cycles/h is considered sufficient to effectively reduce the viral load of OR. Only essential employees are admitted to the OR, movement in/out is limited, and doors must be closed. Use grade III PPE during intubation and extubation. Use proper filters and closed systems for CO2 curettage and non-analectomy There are several important considerations for anal surgery during the COVID-19 pandemic
Some evidence supports fecal-oral transmission of COVID-19. It is important to emphasize that positive pressure anal surgery, such as minimally invasive anal surgery and transanal microsurgery, are aerosol-generating procedures. Therefore, it is appropriate to perform periodic preoperative differential testing for SARS-CoV-2, in addition to nasopharyngeal fluid examination, in patients undergoing transanal surgery under positive pressure. For patients with confirmed SARS-CoV-2 infection, conventional robotic and open approaches may be safer alternatives when surgery cannot be postponed.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References Chebli JMF, Queiroz NSF, Damião AOMC, Chebli LA, Costa MHM, Parra RS. How to manage inflammatory bowel disease during the COVID-19 pandemic: A guide for the practicing clinician. World J Gastroenterol 2021; 27(11): 1022-1042 [PMID: 33776370 DOI: 10.3748/wjg.v27.i11.1022]