This is an automatically translated article.
Posted by Specialist Doctor II Nguyen Trung Thanh - Anesthesiologist - Anesthesiology Department - Vinmec Central Park International Hospital
There is a high risk of a patient being injured by the surgical position. Accordingly, careful assessment of each patient prior to anesthesia is important to reduce the risk of complications related to the surgical position.
1. Nerves for upper extremities
The brachial plexus is formed by the anterior branch of the spinal spinal nerves from neck 5 to thorax 1, located in the axillary fossa. This plexus gives rise to lateral and seven terminal branches that provide sensory and motor control of the upper extremities and the scapula.
2. Upper extremity nerve injuries due to surgical positioning
2.1.Axial Nerve Disease
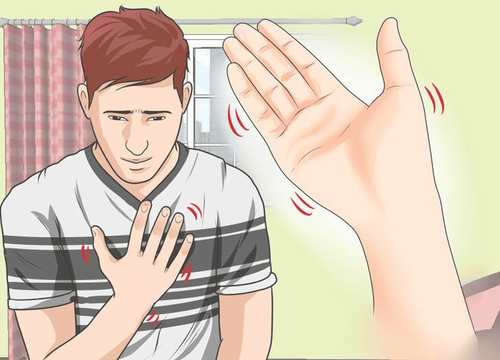
Perioperative ulnar neuropathy is the most common of the upper extremity nerve injuries associated with surgery. Several factors are associated with ulnar nerve disease including direct extrinsic pressure on the nerve, internal compression, and inflammation.
The time of onset of symptoms appeared at least 24 hours after surgery, which suggests that the mechanism of acute trauma occurred mainly outside the operating room. Furthermore, medical patients also develop ulnar neuropathy during hospital stay.
Effects of elbow flexion: The ulnar nerve is the only major peripheral nerve in the body that travels on the extensor side of the joint, specifically the elbow. All other major peripheral nerves differ on the flexor side of the joint (eg, the median and femoral nerve). This anatomical difference may play a role in ulnar neuropathy. In general, peripheral nerves begin to lose function and appear ischemic when they are stretched beyond 5% of their normal length. When the elbow is flexed, especially > 90 degrees, the ulnar nerve is stretched. Prolonged elbow flexion and ulnar nerve strain can lead to ischemia sufficient to cause symptoms in conscious, sedated patients, and long-term damage in all.
Prolonged elbow flexion > 90° increases internal pressure on the nerve and is just as important as extrinsic extension of compression. The ulnar nerve passes posterior to the medial condylar process and runs under the fascia that holds the ulnar carpal flexor tendon and follows this muscle into the anterior forearm region. This fascia extends from the medial condylar process to the elbow process. Bend the elbow, which stretches this fascia, often placing great pressure on the nerve that runs inside.
Arm extension and ulnar neuropathy: Forearm and hand extension does not reduce the risk of ulnar neuropathy. These effects occur on the distal side of the elbow. The supine hand position is often used when positioning the patient's hand to prop the operating table or close to the person to rotate the humerus. That position makes the patient uncomfortable and they will rotate the humerus to increase comfort. External rotation of the arm will reduce the impact on the elbow including the ulnar nerve from the direct forces of the hand or tabletop. This rotation relieves external pressure on the ulnar nerve.
ulnar nerve disease recovers 40% after 5 days, 80% within 6 months if only sensory nerve is damaged. There are very few cases where both motor damage and sensory damage recover within 5 days; only about 20% recover within 6 months and most lead to long-term motor dysfunction and pain. The motor nerve fibers are located between the nerves. Damage to these fibers may be associated with severe ischemia or pressure on all ulnar nerves, and recovery time may be prolonged or impossible.
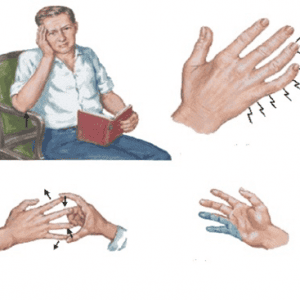
2.2. Medial neuropathy
Medial neuropathy is especially common in men between the ages of 20 and 40. These subjects often have large biceps and reduced flexibility (eg, bodybuilders). Large biceps and reduced flexibility tend to be difficult and prevent full extension of the elbow. This prolonged limitation in range of motion leads to shortening of the median nerve over time.
Medial neuropathy is often associated with movement disorders and is not easily reversible. In fact, over 80% of middle neuropathies have motor dysfunction lasting 2 years from onset.
As noted earlier, the nerve becomes ischemic when stretched > 5% of its length. It twists and ruptures the microvasculature, both of which lead to decreased perfusion pressure.
When the patient is anesthetized for surgery, their elbow is extended enough to rest on the operating table arm or along the torso. Elbow extension leads to median nerve extension and ischemia, usually in the elbow area. Therefore, it is important to provide appropriate forearm support, especially in patients with large, bulky biceps and who are unable to extend their elbows due to lack of flexibility.
2.3. Radial Neuropathy
Radial neuropathy occurs more often than median nerve. The radial nerve appears to be injured by direct compression (as opposed to the median nerve, which is usually stretched). The key factor that appears to be nerve compression occurs in the mid-humeral segment where the nerve rotates behind the bone.
Radial neuropathy tends to have a better recovery than the ulnar and median nerves. About 50% recover well within 6 months, and 70% fully recover after 2 years.
Injury to the brachial plexus: often occurs in patients undergoing mediastinal surgery. The risk of brachial plexus injury in patients undergoing thoracic surgery is particularly high in patients who have used the internal thoracic artery in the internal thoracic bundle to bridge the artery to recirculation. rim of the heart. This finding is thought to be related to excessive concentric contraction of the thorax resulting in the brachial plexus being compressed between the collarbone and the ribs or being stretched. Patients undergoing surgery in the prone and side-lying position are at higher risk than those who are supine.
There are many potential hazards that can occur with the brachial plexus in the prone and side-lying positions. For example, the brachial plexus may be trapped between the ribs and collarbone. Special care should be taken because changing positions can aggravate this problem. For the patient in the prone position, the patient's arms should be placed along the sides of the body if possible. Shoulder flexion >90°, especially for long periods of time, can lead to plexus injury.

3. Other causes of nerve damage in the upper extremities
Pillars to hold Faraboef to help bulge the upper abdomen (in liver surgery) against the closed arm along the patient's torso. The side position with the upper arm resting on the palm rest puts pressure on the soft tissue between the arm and the palmistry. Unsupported arm: medial brachial nerve compression when the elbow of the immobilized arm (beside the patient or the upper operating table arm) is displaced, support is lost, and the weight of the upper limb is placed on mid-bones arm. There are many risks to a patient being injured by the surgical position. It consists of mechanical forces caused by the surgical position leading to soft tissue and nerve damage. The immobilized position can also impair a patient's normal physiological function and should be considered for all patients, especially any position other than the supine position. Careful assessment of each patient prior to anesthesia is important to reduce the risk of complications related to the surgical position.
Department of Anesthesiology and Anesthesia of Vinmec International General Hospital is one of the departments highly appreciated by patients for its professional quality and care services, helping the patient's treatment and recovery process to be effective. the best.
Apply the world's most advanced technology: The world's most advanced epidural analgesia (ESP) pain relief technique; Anesthesia by ultrasound machine, do not use morphine to relieve pain after surgery. The team of leading experts: The doctors are well-trained and experienced, and are members of the Anesthesiology Associations in Vietnam and Europe. Cooperate with leading professors and experts at domestic and international frontline hospitals to exchange techniques and apply the latest methods of anesthesia and pain relief. Professional - comprehensive patient care: patients are fully and fully consulted before anesthesia and analgesia before and after surgery; apply the program of early recovery after surgery for patients; guide appropriate methods of exercise and rehabilitation so that patients can return to normal activities soon.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.