This is an automatically translated article.
Epidural hematoma can increase cranial pressure, seriously affecting the patient's life. The primary treatment of this condition is surgical removal of the epidural hematoma.
1. What is an epidural hematoma?
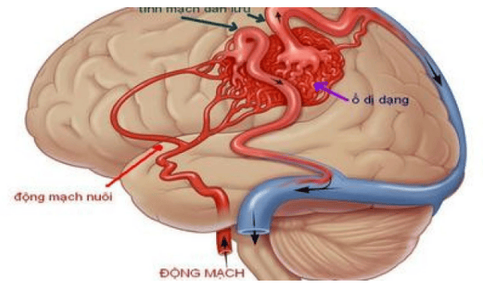
Meninges are membranes that surround the brain in the skull. There are 3 layers of meninges, in which the outermost layer close to the skull is called the dura mater, the innermost layer closest to the brain is called the soft membrane, and the layer between the dura mater and the soft membrane is called the arachnoid membrane. The epidural space is the space between the skull and the dura mater. Because the dura is usually firmly adhered to the inner surface of the skull, the epidural space is a virtual space, present only when there is a tumor or a hematoma between the skull and the dura.
Epidural hematoma is the presence of a hematoma in the epidural space. Epidural hematomas often occur after traumatic brain injury, because the skull fractures tear the dura and damage blood vessels in the brain. These blood vessels bleed and cause a hematoma in the epidural space. Due to the organization of the brain and the cerebrospinal fluid, the blood vessels are located in the skull, which is a closed box with an unchanging volume. The formation and growth of an epidural hematoma will increase intracranial pressure. Increased intracranial pressure will reduce cerebral perfusion pressure, then cause hypoxia due to decreased cerebral perfusion pressure. If not timely intervention, high and prolonged intracranial pressure will cause retraction, jamming of components in the skull through the slits of brain organization, seriously threatening the patient's life.

Chấn thương sọ não là nguyên nhân gây máu tụ ngoài màng cứng
2. Symptoms of epidural hematoma
With an epidural hematoma, the person may lose consciousness at the time of the injury. The classic scenario is that the patient will be unconscious at the time of the injury, followed by a period of wakefulness of several hours, after which symptoms worsen, the patient loses consciousness when hematoma is formed.
However, in many cases, the patient does not lose consciousness after the initial trauma. After regaining consciousness, the person may have symptoms such as drowsiness, severe headache, discomfort, nausea, weakness in one arm or leg, difficulty speaking, or sometimes convulsions. jerk.
Head trauma causing epidural hematoma is a very serious condition, therefore, when an injury occurs, the patient should be urgently taken to the hospital for emergency and timely intervention.
3. Surgery to remove epidural hematoma
When the patient is suspected of having an epidural hematoma, the doctor will perform a physical examination, check the patient's level of consciousness, examine the eyes for signs of increased intracranial pressure, look for signs of hand weakness, leg weakness,... Some imaging techniques such as CT scan of the head, X-ray will be performed to detect epidural hematoma and detect associated injuries if any.
Depending on the patient's condition, the doctor will prescribe appropriate treatment. If the hematoma is small and causes no symptoms, the hematoma may reabsorb on its own. The patient does not need treatment, but only needs to be monitored and taken regularly to ensure that the hematoma does not develop.
If the hematoma is large and there are no contraindications, the patient will be surgically removed the epidural hematoma. Surgical technique to remove epidural hematoma includes steps:
Based on the image of hematoma on CT scan or encephalogram, the surgeon will make a scalp incision, then open or gnaw the skull to near the edge of the hematoma. Identify blood vessels that are flowing to stop bleeding early, use a spoon to remove each part of the hematoma to reduce compression. After the epidural hematoma is removed, the doctor will closely observe the color of the dura. If the dura is dark blue, the patient is likely to have a subdural hematoma. The doctor will open the dura for about 1cm to check, if there is a hematoma, he will conduct a subdural blood draw. Then, the doctor will patch the dura to avoid the passage of cerebrospinal fluid from the arachnoid space to the epidural. Place the drainage tube outside the epidural, close the incision.
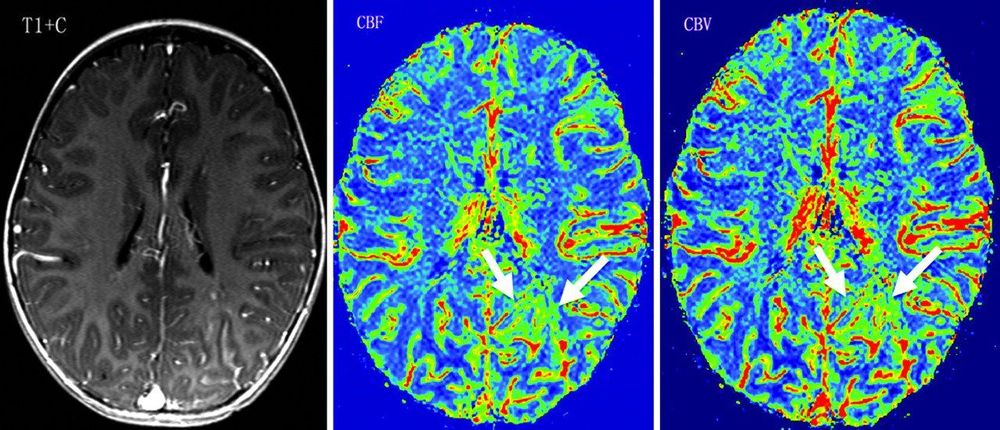
Chụp CT não giúp chẩn đoán máu tụ ngoài màng cứng
4. Possible complications in epidural hematoma surgery
Common complications during surgery to remove an epidural hematoma are hypoxia and hypotension. These are two very dangerous complications that can damage brain cells. To prevent these complications from happening, the anesthesiologist must establish a safe airway, the infusion must be calculated to introduce the correct amount into the body, ensuring the volume of circulation.
After surgery, the patient may have a retracted tongue, increased secretions, the secretions will block the bronchi, which can lead to atelectasis due to hypoventilation. In addition, the patient may have recurrent hematomas at the old surgical site, the hematoma may be missed during surgery, or the lesions appear after surgery. Cerebral edema can also appear, this is a serious and extremely dangerous complication. Therefore, after successful surgery to remove epidural hematoma, it is necessary to actively resuscitate and closely monitor the patient to intervene promptly when the patient has a bad change.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. examination and treatment at the Hospital.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.
SEE MORE
How dangerous is a subdural hematoma after an injury? Chronic subdural hematoma in the elderly Subdural hematoma: Symptoms, diagnosis and treatment