This is an automatically translated article.
The article was written by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalGastric polyps are the cause of some symptoms of stomach and digestive diseases such as abdominal pain, bleeding, indigestion... Gastric polyps are detected during gastroscopy. According to Gastroenterologists, in order to have a healthy digestive system, it is necessary to have a reasonable diet, a healthy lifestyle, and periodic examinations for early detection and appropriate measures.
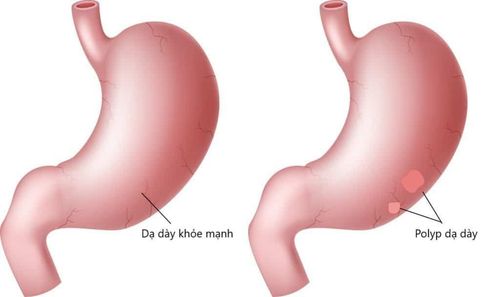
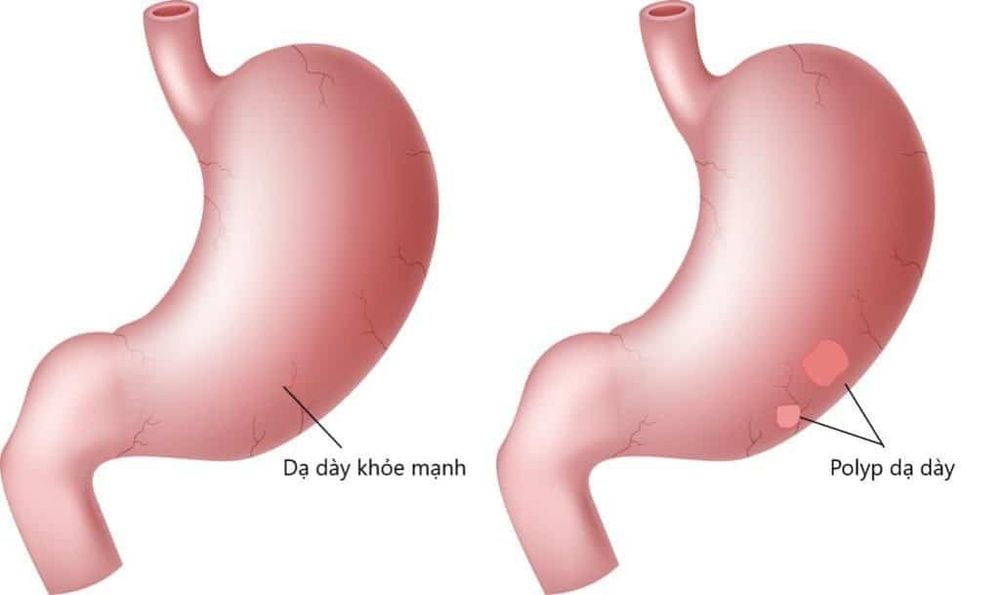
1. What are stomach polyps?
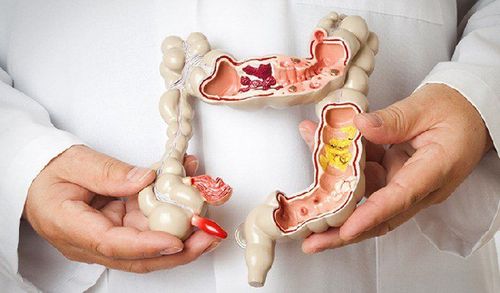
Stomach polyps are raised growths of various shapes (elliptical or circular), with stalks, sometimes called tumors. This tumor is formed due to excessive proliferation of the stomach lining.
With the increasing use of endoscopy, abnormalities that can be seen with the naked eye, such as polyps in the gastrointestinal tract, are encountered more often.
Gastric polyps usually originate in the mucosa but cover a wide range of pathologies, possibly even submucosal or extrinsic. Found in 6% of upper endoscopy cases, gastric polyps are a heterogeneous group of epithelial and subepithelial lesions that may vary in histology, cancerous potential, and management. Although most are asymptomatic (>90%), larger polyps may present with bleeding, anemia, obstruction, or abdominal pain.
Most have no risk of cancer, but there are a small number of polyps with potential for malignancy that require further endoscopic treatment and/or periodic monitoring. These polyps are usually identified histologically because they do not have reliable distinguishing features on endoscopy. Since many gastric polyps have a similar endoscopic appearance, their classification depends on the histological compartments in which they arise (i.e. epithelial, stromal, or mesenchymal).
2. Symptoms of stomach polyps
Gastric polyps usually do not cause specific symptoms. However, stomach polyps enlarge, ulcers can develop on its surface, or rarely, polyps can block the digestive tract between the stomach and small intestine.
If you have stomach polyps, you may experience the following symptoms:
Stomach pain Abdominal pain or pain when pressing the abdomen Bleeding Nausea and vomiting Bloody diarrhea Eating indigestion... Patients should not be subjective when there are symptoms above, which need to be examined and treated early.
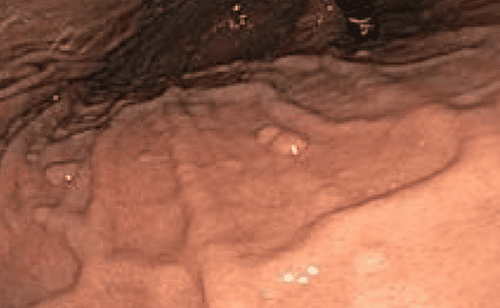
3. Gastroscopy to diagnose gastric polyps
During a gastroscopy, a gastroenterologist or technician inserts a flexible tube with a camera into the mouth and down the throat allowing the doctor to see inside the stomach.This is a common method for high accuracy today to examine and diagnose gastric pathologies and gastric polyps such as:
Early diagnosis of small stomach lesions can also be seen. entire stomach, inner regions of stomach spasmodic, torsional dyskinesia Inflammation of atrophic or hypertrophic gastric mucosa Gastric ulceration Gastroduodenal tumors (benign, malignant, neoplasms, neoplasms) blood vessels, cancer...) Stomach polyps Gastric polyps are removed during endoscopy Combined with biopsies and tests to help diagnose more accurately

4. Methods of treatment
Small polyps that are not adenomas may not require treatment. Polyps usually cause no signs and symptoms and rarely become cancerous.
Instead, a gastroenterologist may recommend periodic monitoring of gastric polyps. You may undergo an endoscopy to see if the stomach polyp has matured. Stomach polyps that grow or show signs and symptoms can be removed.
5. Removal of adenomatous polyps and large gastric polyps
Treatment to remove gastric polyps may be recommended if the gastric polyps are adenomas or if they are larger than 2/5 inches (1 cm) in diameter. Most stomach polyps can be removed endoscopically, a few require surgery to remove the polyps.
6. Stomach polyp syndromes
Cellular polyps are usually mucosa-based but can originate in any of the three embryonic layers. These polyps are the result of disordered growth of local tissues.
Examples include Peutz-Jeghers polyps and juvenile polyps, as well as hamartomatous polyps with no specific name. They may be sporadic in nature or be associated with various multiple polyposis syndromes such as Peutz-Jeghers syndrome, juvenile polyposis syndrome, and Cowden syndrome (PTEN or multiple hamartoma syndrome), to be presented. under.
6.1 Peutz-Jeghers Polyp Syndrome Peutz-Jeghers syndrome is an autosomal dominant disorder with a unique set of findings, including lipomas throughout the gastrointestinal tract and hyperchromia. pigmentation, especially on the lips.
Although patients with this syndrome are more likely to have small bowel or colon polyps, gastric polyps occur in about 15% to 30% of patients. Peutz-Jeghers polyps have a characteristic glandular epithelium with dilated follicular glands, supported by a well-developed smooth muscle skeleton adjacent to the muscular mucosa. In the small intestine and colon, these lesions can be distinguished from juvenile polyps, as Peutz-Jeghers polyps have an intact stroma with a "fan-shaped" appearance of smooth muscle fibers.
However, syndromic gastric polyps are often indistinguishable from nonspecific hyperplastic gastric polyps. Therefore, it is imperative that the pathologist be provided with adequate endoscopic and clinical information to ensure an accurate diagnosis. Furthermore, it should be pointed out that when hamartomatous syndrome is suspected, polyps from the small intestine and colon are more likely to be diagnosed.
6.2 Juvenile Polyps and Juvenile Polyposis Syndrome Juvenile polyps are mucosal tumors consisting mainly of stroma and dilated cystic glands; they are therefore classified as hamartomatous polyps.
They are sometimes called inflammatory polyps or polyps due to the appearance of swollen, mucus-filled glands, inflammatory cells, and edema. Juvenile polyps are usually solitary lesions of the scalp and range in size from 3 mm to 20 mm. When found singly, they are thought to be benign, non-syndromic incidental lesions. However, when multiple polyps are seen in adolescents, juvenile polyposis syndrome should be considered.
As this is a pathological-clinical diagnosis, communicating a complete record of endoscopic and clinical information is essential to the pathologist's success. Juvenile polyps are an autosomal dominant disorder that typically carry a 50% higher lifetime risk of gastric malignancy. Therefore, for juvenile polyposis syndrome, colonoscopy should be performed starting at age 18 and every 3 years thereafter.

6.3 Cowden syndrome Cowden syndrome is a multisystem, autosomal dominant disorder characterized by overgrowth of hamartomatous tissue of all 3 layers of the embryo.
80% of patients have germline mutations of the PTEN tumor suppressor gene. There are several prognostic criteria for the diagnosis of this syndrome, including facial trichilemmomas, keratosis pilaris, and papillomas. As with other clinical-pathological diagnoses, the importance of adequate communication between the endoscopist and the pathologist cannot be overemphasized.
Cowden syndrome has a slight predominance in females and the age of diagnosis is between 16 and 65 years. Transformation of gastrointestinal polyps into malignancy is thought to be extremely rare; Therefore, surveillance endoscopy is not recommended by most.
However, disorders and malignancies of the breast, thyroid and genital tract are more common; therefore, further clinical investigation is needed when this diagnosis is suggested on endoscopic biopsy.

Identification of such polyps requires histological evaluation and may involve additional diagnostic investigation techniques, such as parallel biopsy, immunohistochemical staining, EUS endoscopic ultrasound and EUS-assisted tissue collection.
Furthermore, it is essential that the gastroenterologist provide adequate endoscopic and clinical information to the pathologist for an accurate diagnosis, as many diseases have similar histological features.
Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, gastrointestinal polyps with a high success rate...
Along with that, At Vinmec Hospital, screening for gastric cancer and gastric polyps is done through gastroscopy with an Olympus CV 190 endoscope, with NBI (Narrow Banding Imaging) function. results in clearer images of mucosal pathology analysis compared with conventional endoscopy, detecting atrophic gastritis lesions, gastric polyps, intestinal metaplasia, low-grade gastric dysplasia, and low-grade gastric dysplasia. high, early stage gastric cancer lesions, gastric polyps are at risk of cancer...
Vinmec Hospital with modern facilities and equipment and a team of experienced experts, always dedicated in medical examination and treatment, customers can rest assured with gastroscopy and esophagoscopy services at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
1. Adam Spiegel, DO, Peter Stein, MD, et al. A Report of Gastric Fundic Gland Polyps. Gastroenterol Hepatol (N Y). 2010 Jan; 6(1): 45–48.
2. Weston BR, DJ, Rex DK. The positive predictive value of endoscopic features is considered to be typical of gastric basal adenomatous polyps. J Clin Gastroenterol. Year 2003; 36 : 399–402. [ PubMed ] [ Google Scholar ]
3. Burt RW. Gastric fundus polyp. Gastroenterology. Year 2003; 125 : 1462–1469. [ PubMed ] [ Google Scholar ]
4. Carmack SW, Genta RM, Schuler CM, Saboorian MH. Current characteristics of gastric polyps: A 1-year nationwide study of 120,000 patients. J Gastroenterol. 2009; 104 : 1524–1532. [ PubMed ] [ Google Scholar ]