This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Head of Department of Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
Irritable bowel syndrome (IBS) places a significant burden on healthcare systems worldwide. Therefore, routine colonoscopy is not recommended in patients with irritable bowel syndrome symptoms younger than 45 years of age without warning signs.
1. Should routine colonoscopy be performed in patients with IBS symptoms younger than 45 years of age?
The high prevalence of irritable bowel syndrome greatly affects the care of patients with irritable bowel syndrome. An important aspect is the health and economic burden of unnecessary testing. Colonoscopy is a common test used to confirm the “absence” of pathology that may be causing a patient’s intestinal symptoms, such as IBD, microscopic colitis, or cancer. colon. This test imposes a significant burden on the patient because of lost work time, illness from preparation, effects related to sedation, and direct financial costs.
This impact is compounded because many primary care providers directly request endoscopy before gastrointestinal consultation. Therefore, colonoscopy is one of the most frequent and expensive tests used in the evaluation of irritable bowel syndrome symptoms. Therefore, the authors recommend against routine colonoscopy in patients with irritable bowel syndrome symptoms younger than 45 years of age without warning signs.
2. Consider indications for colonoscopy, colon cancer screening in patients with IBS symptoms over 50 years old
2.1. Consider key patient characteristics when deciding to proceed with endoscopy
First, it is important to consider the key patient characteristics when deciding to proceed with endoscopy – these are known as “alarming features” and include dyspepsia, melena , unintentional weight loss, older age at symptom onset, family history of IBD, colon cancer, or other serious digestive disease. When present, one is more concerned about identifying a pathological process that may be causing the patient's symptoms. However, alarm features in irritable bowel syndrome patients have low predictive value.

2.2. Colon cancer screening is a particular consideration in IBS patients over 50 years of age
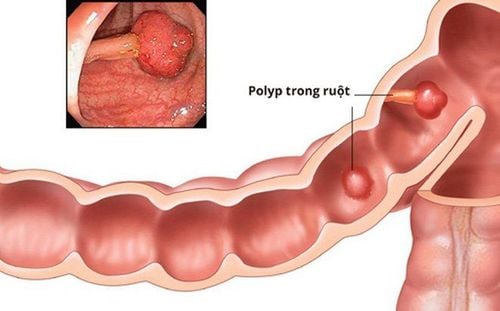
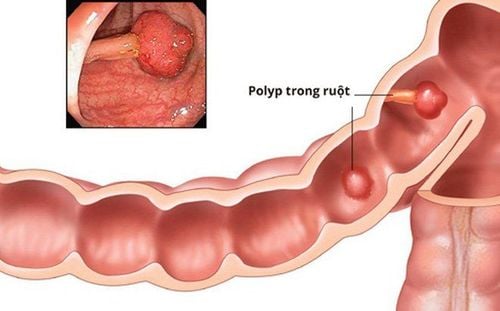
As a second piece of evidence to consider the indication for colonoscopy, colon cancer screening is a special consideration in patients with irritable bowel syndrome. It is important for patients to be up-to-date on colon cancer screening independent of their current irritable bowel syndrome complaints. In other words, if a patient with presumptive Irritable Bowel Syndrome presents to the clinic with Irritable Bowel Syndrome symptoms at age 52 and has never had a colonoscopy to screen for colon cancer, the Endoscopy should be based on the person's age and be considered independent. of irritable bowel syndrome symptoms. Not surprisingly, a colonoscopy is normal. In a large US study, the incidence of colon polyps was lower in irritable bowel syndrome patients than in healthy controls. The reason for this is unclear but does not depend on age.
2.3. Encourage endoscopy in patients with IBS symptoms and no warning signs
Third, colonoscopy has been recommended in patients with irritable bowel syndrome symptoms and no warning signs, as it is thought that pain during colonoscopy may be a measure. aid in the diagnosis of irritable bowel syndrome. This stems from the theory that IBS symptoms represent visceral hypertonia, a concept supported by the higher levels of pain reported in IBS patients compared with IBS. with subjects without irritable bowel syndrome during distention of the colon and rectum. One study found that subjects with irritable bowel syndrome experienced pain during colonoscopy that reproduced their irritable bowel syndrome pain. This has been confirmed by others (age 65) and led investigators to suggest that colonoscopy pain may be an "adjunct" to the diagnosis of irritable bowel syndrome. However, this has never been demonstrated in large-scale and controlled trials and the presence of multiple confounding factors (variation in sedation procedure, quality of preparation, skill of endoscopist and CO2 use) renders this theory unconfirmable.
2.4. Encourage endoscopy in patients with IBS symptoms and no warning signs
Fourth, clinicians expressed concern about important pathological omissions in patients with irritable bowel syndrome symptoms. Several studies have investigated this issue. Chey et al determined that the most common lesions identified in irritable bowel syndrome patients during colonoscopy were hemorrhoids, diverticular disease, and polyps. However, polyps were found in only 7.7% of cases in IBS patients compared with 26.1% in non-IBS patients (P < 0.0001). This still makes sense even after controlling for age and other factors.
In a more recent study of 559 subjects who met the Rome III Irritable Bowel Syndrome criteria, alarm features had a higher detectable incidence, however, even among 136 Subjects had no alarm feature, Crohn's disease was found in 7.4% of subjects and celiac disease in 2.9%. This second study may speak to both the poor specificity of the Rome criterion, which has a positivity rate of only 3.35, and the geographic prevalence of diseases such as IBD and CD in the study. carried out in the northern population groups.
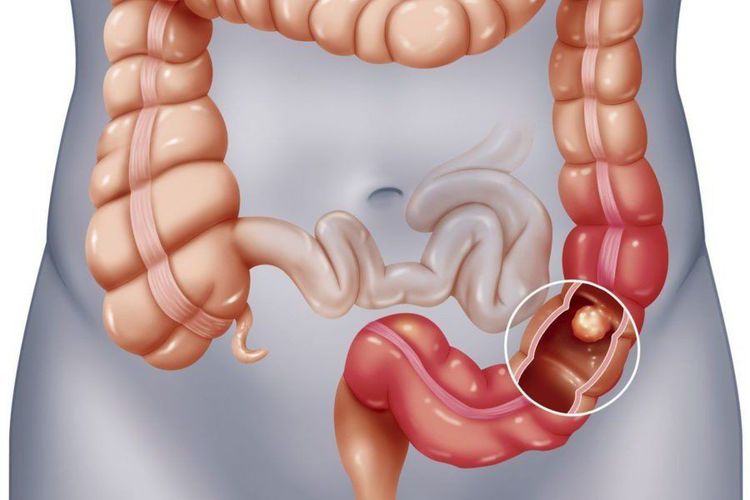
Finally, in the largest study to date from Japan of 4,528 subjects undergoing colonoscopy, 5 colonic tumors were identified in 203 positive irritable bowel syndrome subjects in Rome. However, all were detected in subjects over 50 years of age. None of the subjects had irritable bowel syndrome under 49 years of age.
A common indication used to “justify” colonoscopy in patients with suspected irritable bowel syndrome-D (irritable bowel syndrome with diarrhea) is to “rule out microscopic colitis.” body”.
This may be a particular case in women over 60 years of age who are at high risk for new-onset microscopic colitis. However, data is limited here. Making things even more complicated, a recent meta-analysis identified limitations of the Rome criterion as 32.5% of patients with microscopic colitis would meet the Rome criteria for bowel syndrome. -D stimulus while others met the Rome criteria for functional diarrhea.
3. Conclusion
Based on current evidence, in the absence of alarm features, there seems to be no reason for routine colonoscopy in irritable bowel syndrome subjects younger than 45 years (although out of scope). Because of the scope of this manuscript, the change in screening to age 45 is controversial, and readers are referred to social guidelines and recent publications for a comprehensive review of the topic). In patients older than 45 years, recent negative colonoscopy for colon cancer screening or for other investigative purposes will minimize the need for another colonoscopy for irritable bowel syndrome symptoms. prefer in the absence of new alarm features. In patients considered to be at high risk for microscopic colitis (older age [>60], female sex, and more severe diarrhea), there may be more evidence to support the use of this method. Endoscopic.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Lacy, Brian et al. ACG Clinical Guidelines: Management of Irritable Bowel Syndrome. American Journal of Gastroenterology: January 2021 - Volume 116 - Issue 1 - p 17-44