This is an automatically translated article.
Article written by Dr. Bui Thi Hang, High-tech Unit for Treatment of Cerebral Palsy and Autism - Vinmec Times City International Hospital
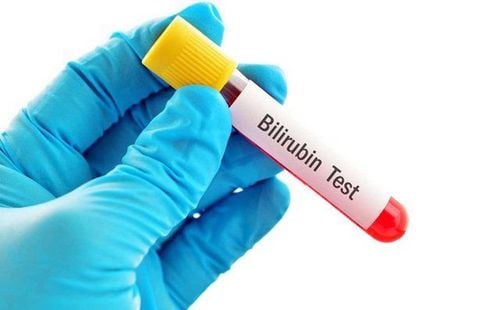
Congenital biliary atresia in neonates is a very difficult disease to diagnose and can only be identified through screening. Currently, there are two methods of screening for congenital biliary atrophy that are proposed by medical experts, namely to test the serum bilirubin level directly in jaundiced children and to use stool cards to screen.
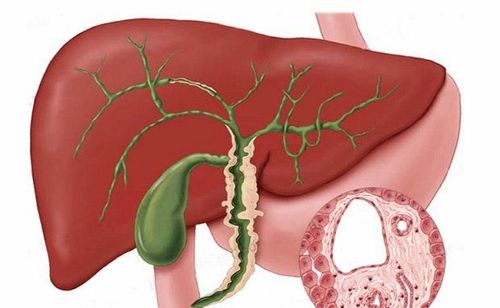
Congenital biliary atresia is the most common cause of end-stage liver disease in children and the leading indication for liver transplantation in children.
Symptoms of biliary obstruction in infants appear a few weeks after birth. Early diagnosis and successful biliary drainage are associated with increased survival compared with children without surgery. However, non-obstructive jaundice is very common in neonates and it is difficult to identify the small number of children with obstructive jaundice. Newborns with biliary atresia present with jaundice and pale stools within the first few weeks of life, this condition is the result of sclerosing inflammation leading to extrahepatic biliary obstruction so that bile cannot pass from the liver to the intestines. . Biliary obstruction leads to liver failure within a year and death within 2 years without a liver transplant.

Education about the importance of early identification of biliary obstruction and finding ways to screen for early neonatal obstructive jaundice is extremely important.
Congenital biliary atresia is difficult to diagnose. Newborns with biliary insufficiency usually look as healthy as other normal infants. However, infants present with jaundice at birth or shortly thereafter and may be clinically indistinguishable from infants with indirect hyperbilirubinemia due to other causes such as “physiological jaundice” and “jaundice”. by breast milk”. or other less common causes such as toxoplasmosis, rubella, cytomegalovirus, herpes and hepatitis B and genetic disorders, such as Alagille syndrome, antitrypsin a-1 deficiency...
Need to consider the diagnosis biliary atresia in any infant presenting with elevated serum direct bilirubin levels and pale stools or decreased biliary excretion.
Currently, there are two methods of screening for congenital biliary atrophy that are proposed by medical experts, namely to test for direct bilirubin concentration in the serum of children with jaundice and to use stool cards to screen. Both methods showed no significant harm to the neonate. A test for total and direct bilirubin levels may be suggested at the time of collection of other blood tests prior to discharge from the maternity ward.
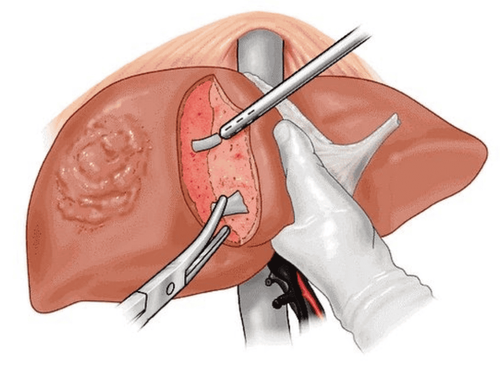
The child has a liver ultrasound to evaluate the presence and size of the gallbladder and to identify any abnormal findings in the hepatobiliary tract, as well as to identify a biliary cyst.
A second potential screening method that has also been studied and used in many countries is to use the fecal tag screening method used in some countries such as Taiwan, Japan...
Sieve Stool color card screening can avoid the need for blood testing in children, but it is often subjective and must be discussed with the child's parents by the physician to determine the color of the stool. Stool miniaturization progresses over time so there is no set time to start and end screening. Parents need to monitor the baby's stool color continuously daily for the first few months after birth
Below is an image of the infant stool color card used to screen for congenital biliary atresia in children in Taiwan (Pediatrics April 2006, 117 (4) 1147-1154; DOI: doi.org/10.1542/peds.2005-1267) Parents will monitor their child's stool color from the time the baby is released from the maternity home and returns. home. If the child has stool color similar to the picture from 1 to 3 (silver, clay color or light yellow), then the child may have congenital biliary atresia, need to take the child immediately to a medical facility for examination. Or regardless of the color of the child's stool, take the child to the medical facility for examination on the 30th day of age, if the child cannot go to the medical facility for examination, the parents can send the card this stool to medical facilities
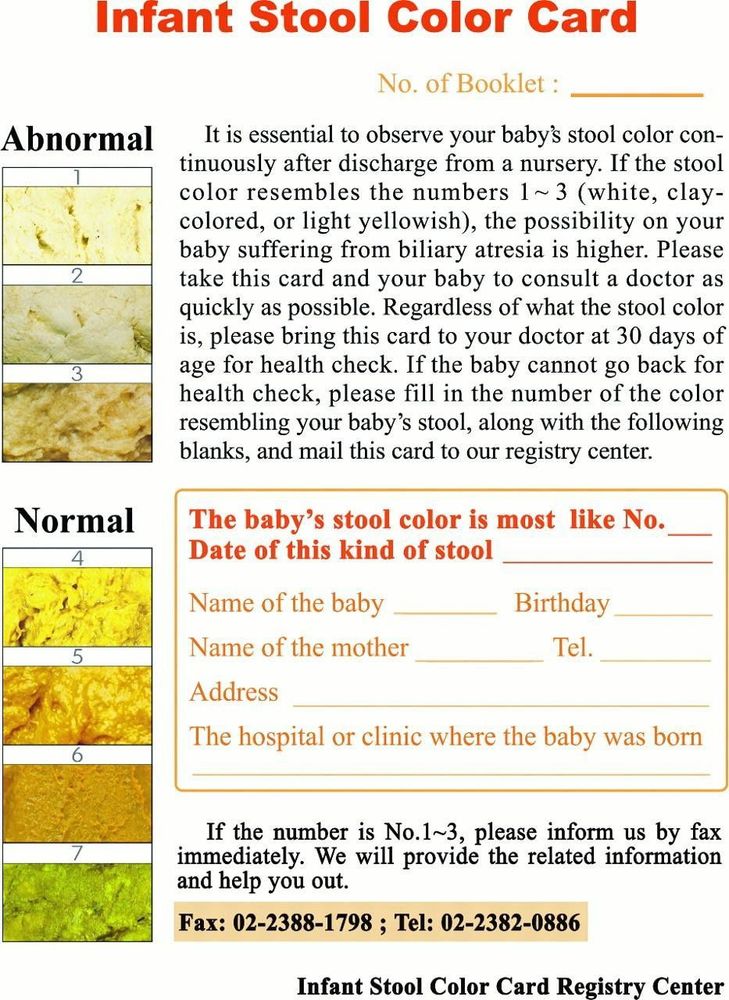
In Vietnam, mothers can completely apply the above screening methods to detect cholestatic jaundice early. If the child has jaundice lasting > 2 weeks (besides the physiological jaundice stage or has stool color in groups 1, 2, 3 as shown above, you need to take the child to a medical facility immediately for examination.
To protect your baby's health, you should perform newborn screening for newborns to detect health problems early.At Vimec, postpartum screening is part of the Maternity Packages. When choosing Package Maternity, pregnant women can:
The pregnancy process is monitored by a team of highly qualified doctors Regular check-ups, early detection of abnormalities Maternity package help facilitate the birthing process Newborns are taken care of comprehensively
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Newborn Screening for Biliary Atresia, Kasper S. Wang, MD, FAAP, FACS, Pediatrics. 2015 Dec; 136(6): e1663–e1669.
doi: 10.1542/peds.2015-3570
Screening for Biliary Atresia by Infant Stool Color Card in Taiwan, Shan-Ming Chen, Mei-Hwei Chang, Jung-Chieh Du, Chieh-Chung Lin, An-Chyi Chen, Hung- Chang Lee, Beng-Huat Lau, Yao-Jong Yang, Tzee-Chung Wu, Chia-Hsiang Chu, Ming-Wei Lai, Huey-Ling Chen and ; the Taiwan Infant Stool Color Card Study Group, Pediatrics April 2006, 117 (4) 1147-1154; DOI: https://doi.org/10.1542/peds.2005-1267