This is an automatically translated article.
The article is written by Master, Doctor Mai Vien Phuong - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
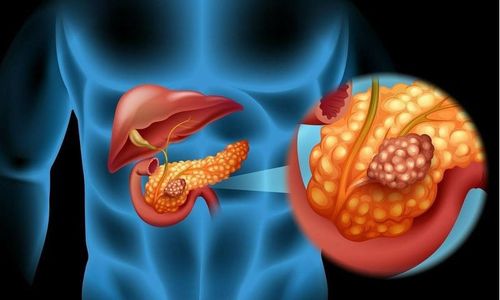
Autoimmune pancreatitis is one of the human autoimmune diseases. Autoimmune pancreatitis was only recently discovered (previously often confused with other conditions), a finding that now plays an important role in making treatment more effective.
1. Overview of autoimmune pancreatitis
Autoimmune pancreatitis is a unique form of the chronic inflammatory disorder of the pancreas, which is precipitated by autoimmune reactions. Autoimmune pancreatitis is classified into 2 types, more than 95% of cases of autoimmune pancreatitis are either manifestations of pancreatic disease or associated with systemic immunoglobulin G4 (IgG4-RD).
Autoimmune pancreatitis and IgG4-RD are recently established disease entities proposed by rheumatologists and gastroenterologists. As awareness and recognition of these disorders by physicians increase, the number of patients diagnosed with autoimmune pancreatitis and IgG4-RD is increasing. Therefore, the clinical manifestations, immunological formation of autoimmune pancreatitis and IgG4-RD are attracting much attention of doctors and researchers.
2. Role of IgG4-RD
IgG4-RD found most commonly in elderly men, it is characterized by marked elevation of serum IgG4 antibody (Ab) and accumulation of IgG4 Ab secreting plasma cells in damaged organs. Another important feature of IgG4-RD is its multi-organ involvement, this disorder heavily affecting the pancreas, bile ducts, lungs, salivary glands, and kidneys.
Autoimmune pancreatitis is a manifestation of pancreatic IgG4-RD. Elevated serum levels of IgG4 Ab are widely used as a diagnostic marker for autoimmune pancreatitis and IgG4-RD. In addition, patients with multiple organ involvement of IgG4-RD had higher serum IgG4 Ab levels, suggesting that measuring serum IgG4 levels is not only useful for diagnosis but also assess disease activity.
However, it should be noted that the level of this IgG subtype is not always considered a perfect biomarker for diagnosis, evaluation of activity in autoimmune pancreatitis and IgG4-RD. In fact, serum IgG4 Ab levels are significantly elevated in a significant fraction of patients with pancreatic cancer, about 20% of patients with autoimmune pancreatitis have normal serum IgG4 Ab levels. Furthermore, patients with autoimmune pancreatitis sometimes relapse even when they have normal serum IgG4 Ab levels. Therefore, it is necessary to identify other biomarkers that may be useful for the diagnosis and assessment of disease activity in autoimmune pancreatitis and IgG4-RD.
3. Pathogenesis of autoimmune pancreatitis and IgG4-RD
Role of adaptive immunity Autoimmune pancreatitis and IgG4-RD are characterized by an enhanced IgG4 Ab response; therefore, the immune microenvironment that leads to IgG4 Ab production may be involved in the development of these disorders. Various differentiated T-cell subpopulations participate in the enhanced IgG4 Ab response. Effector T cells include type 2 helper T cells (Th2), regulatory T cells (Tregs), follicular helper T cells (Tfh), and cytotoxic CD4+ T cells (CD4+) CTL). Cytokines are produced by subpopulations of T cells, which act to promote the production of IgG4 Ab by B cells.

Role of Interleukin Interleukin-4 (IL-4), IL-10 and IL-13 secreted by Th2 cells and/or Tregs in promoting IgG4 Ab production by healthy control B cells in vitro . In fact, the expression of IL-10, IL-13, and transforming growth factor-β1 (TGF-β1), also induced by Th2 and/or Tregs, was found in the livers of patients with IgG4-RD was higher than in patients with other autoimmune biliary tract diseases. Furthermore, the cytokine responses seen in IgG4-RD were accompanied by enhanced expression of fork-head box P3 (FOXP3), an important transcription factor for Tregs. Koyabu et al. reported that the number of Tregs correlated with IgG4+ cells in the liver of IgG4-RD patients.
4. Th2 and Tregs cells are implicated in the development of autoimmune pancreatitis and IgG4-RD
Along with the enhanced expression of Th2 and Treg-related cytokines in the liver, patients with IgG4-RD have higher expression of Th2 cytokines and chemokines such as IL-4, IL-5, IL-10, CC motif chemokine ligand 17 (CCL17) and CCL22 in salivary glands compared with levels of these molecules in healthy subjects and with Sjogren's syndrome. Such enhanced Th2 responses in the salivary glands are accompanied by the production of TGF-β1 and the accumulation of FOXP3+ Tregs. These data support the idea that Th2 and Tregs cells are involved in the development of autoimmune pancreatitis as well as IgG4-RD. Given that Tregs are potent negative regulators of autoimmune responses, it is possible that Tregs activation is indicative of persistent strong inflammation rather than a component of inflammation in autoimmune pancreatitis and IgG4- RD.
Tfh cells, which express B6 cell lymphoma (BCL6), CXC chemokine receptor type 5 (CXCR5) and produce IL-21, play important roles in germinal center responses. Expression levels of BCL6, CXCR5 and IL-21 in ectopic germinal centers in the salivary glands were significantly higher in patients with IgG4-RD than in patients with Sjogren's syndrome. Tfh cells isolated from the salivary glands and peripheral blood of patients with IgG4-RD have a greater ability to stimulate the production of IgG4 Ab by B cells than tonsil Tfh cells. Percentage of circulating Tfh2 cells, defined as CXCR5 +CXCR3 - CC chemokine receptor type 6 - cells, were positively correlated with serum IgG4 levels in patients with IgG4-RD. Thus, these data support the idea that Tfh cells participate in immunoformation of IgG4-RD through induction of germinal center response. However, the role of Tfh cells in autoimmune pancreatitis remains unclear.
5. Role of CD4 + CTL
CD4+CTL is a unique subpopulation of effector T cells commonly seen in patients with chronic viral infections. CD4 + CTL is localized in the salivary glands of patients with IgG4-RD. These cells express T-box-express-in-T-cells (T-bet) and produce interferon-g (IFN-γ). Although both Th1 and CD4+CTL cells express T-bet and IFN-γ, they differ in the expression levels of the myeloid cell marker (CD11b) and the ability to produce CCL4 and IL-1β. In addition, these cells produce several cytotoxic proteins, including perforin and granzyme. More importantly, these cells secrete TGF-β1, one of the pro-fibrinogenic protozoan factors. Thus, CD4+CTL is involved in chronic fibroinflammatory responses associated with IgG4-RD. However, the accumulation of CD4 + CTLs has not yet been verified in the pancreas of patients with autoimmune pancreatitis.
6. Innate immunity
Innate immunity is one of the main defense mechanisms of the host against microbial infections. Recognition of microbial components by Toll-like receptors (TLRs) and nucleotide-linked oligomerization domain-like receptors (NLRs) induces a proinflammatory cytokine response to rule out microbial infections. object. It has been well established that excessive innate immune responses underlie different types of autoimmune disorders. Recent studies have highlighted the importance of innate immunity in autoimmune pancreatitis and IgG4-RD
7. Role of innate immunity in the development of autoimmune pancreatitis and IgG4-RD
Many authors have mentioned the role of innate immunity in the development of autoimmune pancreatitis and IgG4-RD. The authors initially examined whether peripheral blood mononuclear cells (PBMCs) isolated from IgG4-RD patients produced inflammatory cytokines upon exposure to the TLR ligand. They found that they secreted more IgG4 Ab and Th2 cytokines than PBMCs from healthy controls.
In subsequent studies, the authors used a co-culture system, consisting of peripheral blood CD14 + mononuclear cells, CD19 + B cells, CD3 + T cells isolated from the patient. autoimmune pancreatitis and IgG4-RD. This co-culture system allowed the authors to demonstrate that B cells produce large amounts of IgG4 Ab in the presence of NLR and TLR ligands when co-cultured with isolated mononuclear cells from patients with autoimmune pancreatitis as well as with IgG4-RD, but not with mononuclear cells from healthy controls.
8. Role of monocytes in autoimmune pancreatitis
Interestingly, peripheral blood mononuclear cells isolated from patients with autoimmune pancreatitis and IgG4-RD, effectively induced IgG4 Ab production by B cells from the subjects. healthy controls in a T-cell-independent manner. TLR and NLR stimulation leads to the production of B-cell activating factor (BAFF), which induces an IgG4 Ab response. In addition to monocytes, peripheral blood basophils isolated from patients with autoimmune pancreatitis and IgG4-RD also promote IgG4 Ab production by B cells from healthy controls in an independent manner. into T cells, BAFF. These pioneering studies fully support the concept that excessive innate immune responses are involved in the development of autoimmune pancreatitis and IgG4-RD. Indeed, the expression of TLRs was verified in the salivary glands and pancreas of patients with autoimmune pancreatitis and IgG4-RD.
In summary, autoimmune pancreatitis and IgG4-RD are newly established disease entities. Both of these disorders are characterized by elevated serum IgG4 Ab levels and accumulation of IgG4-expressing plasma cells in the affected organs. Furthermore, the induction of remission by prednisolone was accompanied by a marked decrease in serum IgG4 Ab levels in patients with autoimmune pancreatitis à IgG4-RD. Therefore, the serum level of this IgG subclass is certainly a useful biomarker for both diagnosis and assessment of disease activity.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Hara A, Watanabe T, Minaga K, Yoshikawa T, Kamata K, Kudo M. Biomarkers in autoimmune pancreatitis and immunoglobulin G4-related disease. World J Gastroenterol 2021; 27(19): 2257-2269 [DOI: 10.3748/wjg.v27.i19.2257]